Kyra Zens
E-CDC risk status: endemic
(last edited in May 2025, update for 2024: 435 reported cases)
History and current situation
Tickborne Encephalitis (TBE) was first reported in Switzerland in 1969.1 From the 1970s through the 1990s the causative agent, the tickborne encephalitis virus (TBEV), was found to be endemic in geographically localized areas within the northeastern part of the country.2-4 A formal case definition and surveillance activities were introduced in 1984 and TBE was made a mandatory notifiable disease in 1988.5 Currently, all suspected TBE cases are reported to the Swiss Federal Office of Public Health (FOPH) using a two-tiered system. First, all laboratory tests indicative of acute TBEV infection are reported to the FOPH. Then, attending physicians are requested to complete a notification form providing specific clinical information, which is forwarded to the cantonal physician for review and then returned to the FOPH (Table 1). Both laboratory and completed clinical reporting forms are registered and maintained by the FOPH.5 The TBE case definition used in Switzerland is based on a combination of clinical and laboratory criteria and is similar to, but differs slightly from, that used by the ECDC in that “possible” cases, in addition to “probable” and “confirmed” cases, are included (Table 1).6-9
The majority of TBE cases in Switzerland are reported between April and October (Figure 1).10 Cases are more commonly reported in men, compared to women, and individuals aged 50-69 are most affected, though a bimodal trend with a smaller peak in cases among children aged 5-9 is also observed (Figure 2).10 Recent work has demonstrated that approximately 5% of unvaccinated individuals throughout the country are seropositive, suggesting that exposures far outnumber clinically confirmed cases of disease.11 Among clinical TBE cases, approximately 75% recalled a tick bite within the 4 weeks prior to disease onset.6,8 Approximately 75% result in hospitalization. Meningitis is observed in 19-49% of cases,6,12,13 meningoencephalitis in 43-59% of cases,6,12,13 and meningoencephalomyelitis and/or radiculitis in 5-7%.6,12,13 Just under 1% of cases are fatal (Table 1).6,8,13
Over the last two decades, both the geographic range and total incidence of TBE cases have increased dramatically throughout Switzerland.10,14,15 From an initial localization to the northeastern part of the country, TBE cases have increasingly been reported further west- and southward. This has been paralleled by increases in the range of TBEV-infected ticks16-23 and small and large mammal populations with positive anti-TBEV serology (Table 1).24-28 Currently, TBEV has been identified in ticks from most regions of Switzerland and in Liechtenstein, and, accordingly, human cases are now found in most areas of the country.29 In 2020, the nationwide average disease incidence exceeded the WHO’s definition of “highly endemic”, with greater than 5.0 cases/100,000 individuals reported.10
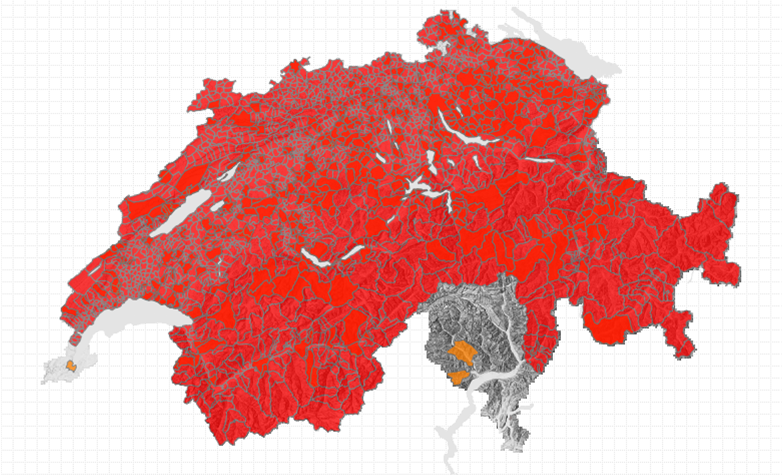
Official recommendations for vaccination against TBE have been in place in Switzerland and Liechtenstein since 2006; initially for all individuals aged 6 and older living or spending significant time in 71 “high risk” areas throughout both countries (Table 1).30 These risk areas, based on reported cases and viral surveillance in the environment, were updated and expanded annually to reflect the changing epidemiology of the disease.29,31 The resulting risk area map (Figure 3) was used until 2018 to define TBE vaccination recommendations throughout the country.29,31 However, in 2019, in view of the continuing increases in incidence and geographic range of disease, health authorities in Switzerland and Liechtenstein expanded the risk area and simplified the vaccination recommendation to cover the entirety of both countries – with the exceptions of the Swiss cantons of Geneva and Ticino14,29 (Figure 3a – 3c). In 2024 the recommendation was further revised to include the canton of Geneva (from summer 2024) as well as to recommend vaccination beginning at 3 years of age.32
Vaccination is reimbursed by compulsory health insurance for individuals to which the recommendation applies; namely those 3 years of age and older living or spending significant time in risk area.14,32 In children 1–2 years of age, vaccination is considered and reimbursed on a case-by-case basis.14,32 Considerations are also made for those with “high risk” occupations, though the cost of vaccination is to be reimbursed by the employer (Table 1).14,32 Nationwide, between 2020 and 2022, just 2% of 2-year-olds were vaccinated, increasing to 50% coverage among 8- and 16-year-olds. Among adults, from the most recent data in 2018, 42% had received at least one TBE vaccine dose while 33% had completed at least the three dose primary series (Table 1).33 Following completion of primary immunization, Switzerland has a unique recommendation for administration of booster vaccine doses every 10 years,30,34 unlike most other European countries and in contrast to the label. However, recent epidemiologic studies in the country have demonstrated that vaccine effectiveness (VE) remains high in both children35 and adults36 over this interval, with sustained protection for at least 10 years after the last vaccine dose was received.
Overview of TBE in Switzerland
| Table 1: TBE in Switzerland | |
|---|---|
| Viral subtypes, distribution | Only the European subtype has been described17,20,22,23 |
| Reservoir animals | Small mammals, generally rodents (Apodemus flavicollis, A. sylvaticus, Myodes glareolus), are the primary reservoir hosts for TBEV observed in Switzerland24 TBEV-infected ticks have also been found on migrating birds21 |
| Infected tick species (%) | Only Ixodes ricinus ticks described; Prevalence in ticks is focal and ranges widely, generally less than 1% of questing ticks but as high as 14.3%16-23,25,26,37 |
| Dairy product transmission | Not documented, risk estimated to be low38 |
| Case definition used by authorities | Possible Case: positive IgM serology with influenza-like illness (ILI) or non-specific neurological signs & symptoms, OR, positive IgM + positive IgG serology without specific clinical symptoms Probable Case: positive IgM serology with meningitis, meningoencephalitis, encephalomyelitis or radiculitis, OR, positive IgM + positive IgG serology with influenza-like illness (ILI) or non-specific neurological signs & symptoms Confirmed Case: positive IgM + positive IgG serology with meningitis, meningoencephalitis, encephalomyelitis or radiculitis, OR, TBE-RNA detection by PCR with meningitis, meningoencephalitis, encephalomyelitis or radiculitis |
| Completeness of case detection and reporting | Case reporting assumed to be complete or near complete due to two-tiered system5-8, though no specific studies have evaluated this |
| Type of reporting | A mandatory notifiable disease since 1988 with reporting to the Swiss FOPH following a two-tiered system:5-8 -First, all laboratory tests positive for evidence of acute TBE are reported -Afterwards, attending physicians are requested to complete a specific notification form providing specific clinical information |
| Other TBE-surveillance | Not routine Studies assessing TBEV in ticks16-23,25,26,37 Studies assessing seropositive blood donors11 |
| Special clinical features | In children:35 -No neurologic involvement reported in 13% of cases -Meningeal irritation, meningitis observed in 35% of cases -Meningoencephalitis in 49% of cases -Encephalitis, encephalomyelitis, radiculitis, paresis reported in 3% of cases In adults: -Hospitalization observed in 71-75% of reported cases6,8,13 -Meningitis in 19-49% of cases6,12,13 -Meningoencephalitis in 43-59% of cases6,12,13 -Meningoencephalomyelitis/Radiculitis in 5-7% of cases6,12,13 -Slightly under 1% of cases are fatal6,8,13 |
| Licensed vaccines | Encepur N® (Bavarian Nordic) Adult Formulation39 Encepur N® Kinder (Bavarian Nordic) Pediatric Formulation39 FSME-Immun® (Pfizer) Adult Formulation40 FSME-Immune® Junior (Pfizer) Pediatric Formulation41 |
| Vaccination recommendations | Localized recommendations based primarily on area of residence since 200630; in 2019 and 2024 the recommendation was expanded to cover all of Switzerland and Liechtenstein with the exceptions of Geneva and Ticino14,29,32 Vaccination is reimbursed by compulsory health insurance for individuals covered by the recommendation: -Individuals 3 years of age and older living or spending significant time in risk areas14,32,33 -In children 1–2 years of age vaccination is considered and reimbursed on a case-by-case basis14,32,33 -For individuals with “high risk” occupations, costs of vaccination are covered by the employer14,32,33 |
| Vaccine uptake | In children34,43 – Average national vaccination uptake (3+ doses) 2019-2022: -2 years old: 2.3% (1.8-2.9) -8 years old: 48.7% (46.9-50.6) -16 years old: 50.1% (48.3-52.0) In adults35 – Average national vaccination uptake (3+ doses) 2018: -18-39 years old: 34.7% (31.5–38.0%) -40-59 years old: 31.3% (29.0–33.8%) -60-79 years old: 32.4% (30.1–34.8%) |
| National Reference center for TBE | Nationales Referenzzentrum für durch Zecken übertragene Krankheiten (NRZK; National Reference Centre for Tick-borne Diseases) Website: www.swissticks.ch The reference center consists of two partners: Institut für Mikrobiologie des Centre Hospitalier Universitaire Vaudois (CHUV) Rue du Bugnon 48 1011 Lausanne Tél. +41 21 314 46 48 / +41 21 314 40 56 (secrétariat) Tél. +41 21 314 49 79 (Prof. G. Greub) Mail: gilbert.greub@chuv.ch ADMED Microbiologie Boucle de Cydalise 16+2300 La Chaux-de-Fonds Tél. +41 32 967 21 01 Mail: admed.microbiologie@ne.ch |
Figure 1: Number of reported TBE cases in Switzerland, 2000 – 2023. Update for 2024: 435 reported cases.
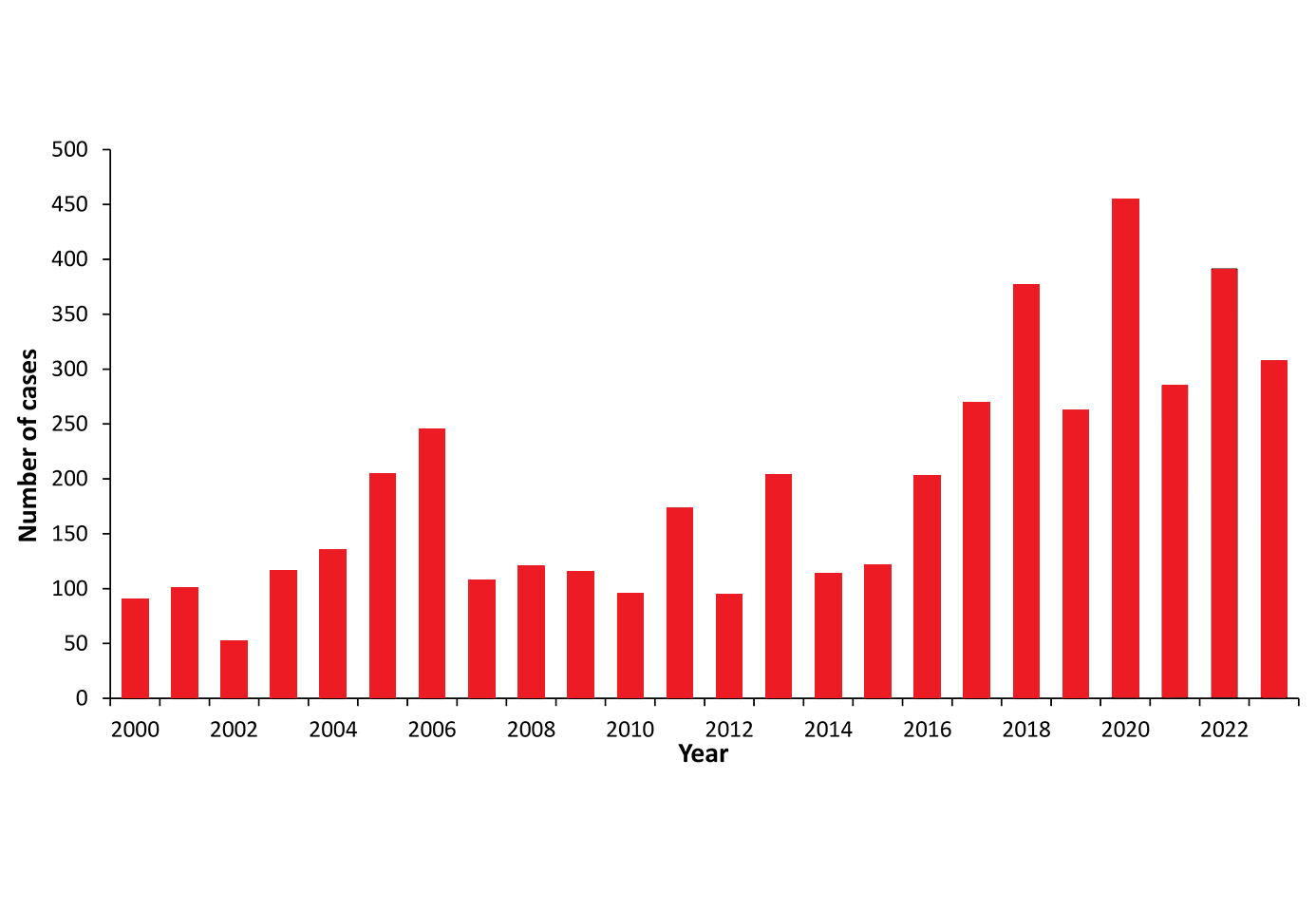
| Year | Number of Cases | Incidence / 105 |
|---|---|---|
| 2000 | 90 | 1.24 |
| 2001 | 100 | 1.37 |
| 2002 | 52 | 0.70 |
| 2003 | 116 | 1.56 |
| 2004 | 135 | 1.81 |
| 2005 | 204 | 2.72 |
| 2006 | 245 | 3.24 |
| 2007 | 107 | 1.40 |
| 2008 | 120 | 1.55 |
| 2009 | 115 | 1.44 |
| 2010 | 95 | 1.20 |
| 2011 | 173 | 2.17 |
| 2012 | 94 | 1.16 |
| 2013 | 203 | 2.48 |
| 2014 | 113 | 1.37 |
| 2015 | 121 | 1.42 |
| 2016 | 202 | 2.39 |
| 2017 | 269 | 3.16 |
| 2018 | 376 | 4.38 |
| 2019 | 262 | 3.03 |
| 2020 | 454 | 5.11 |
| 2021 | 285 | 3.25 |
| 2022 | 388 | 4.38 |
| 2023 | 307 | 3.47 |
| 2024 | 435 |
Figure 2: Age and gender distribution of TBE cases in Switzerland 2000–2023
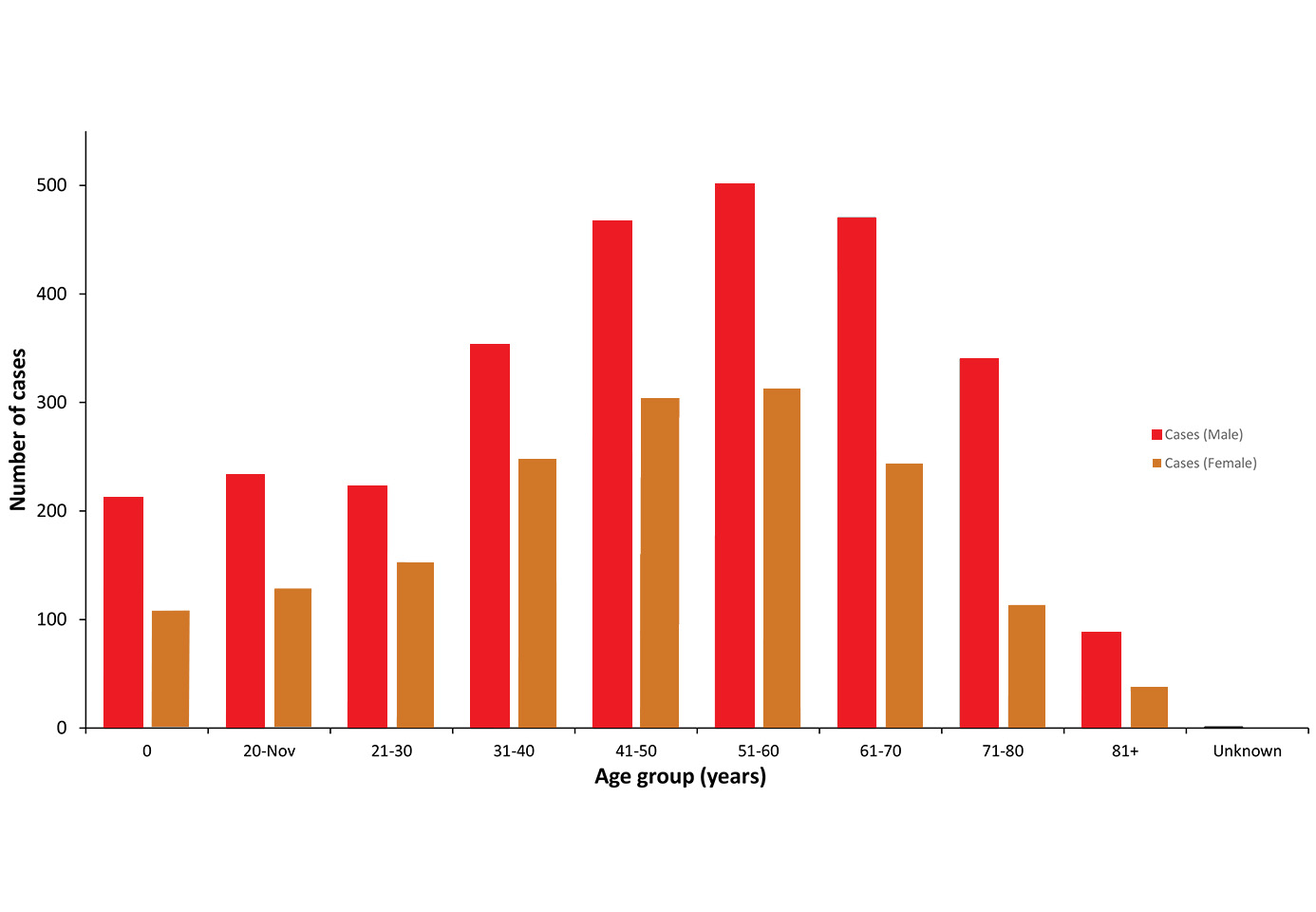
| Age Group (Years) | Cases (Male) | Cases (Female) | (Unknown) |
|---|---|---|---|
| 0-10 | 212 | 108 | 0 |
| 11-20 | 233 | 128 | 2 |
| 21-30 | 222 | 153 | 0 |
| 31-40 | 353 | 248 | 0 |
| 41-50 | 466 | 304 | 2 |
| 51-60 | 501 | 313 | 1 |
| 61-70 | 470 | 244 | 1 |
| 71-80 | 340 | 113 | 0 |
| 81+ | 88 | 38 | 0 |
| Unknown | 1 | 0 | 0 |
Data includes all possible, probable, and confirmed cases according to Swiss TBE case definitions
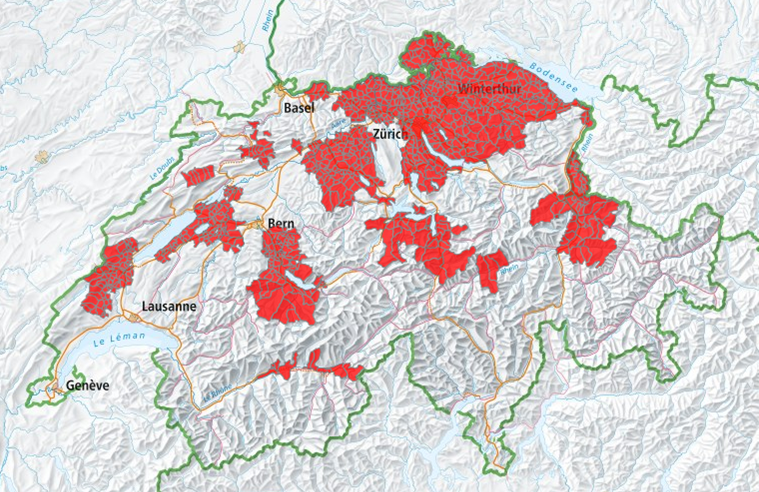
Figure 3a: TBE cases – reported exposure sites, 2012-2023
Latest update available at: https://s.geo.admin.ch/727304e0f5
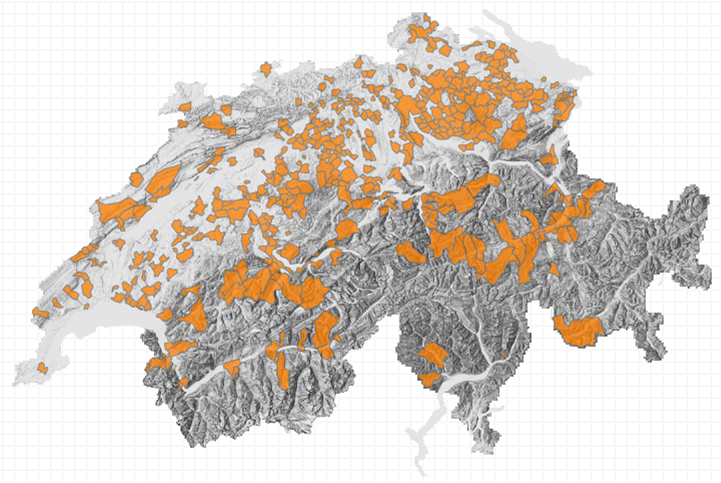
Figure 3c: Extended risk areas where TBE vaccination was recommended, 2019-2023. Risk areas were further extended for all individuals (residents and visitors aged 3+ years) with the exception of canton Ticino, from April 2024
Official update of map not yet available by April 30, 2024 but can be found afterward with latest update at: https://s.geo.admin.ch/727304e0f5
Acknowledgments
Unpublished data were kindly provided by Annora Mack and Ekkehardt Altpeter, Federal Office of Public Health FOPH, Division of Communicable Diseases, Bern, Switzerland.
Author
Contact
Kyra Zens
zens@immunology.uzh.ch
Citation
Zens K. TBE in Switzerland and Liechtenstein. Chapter 13. In: Dobler G, Erber W, Bröker M, Chitimia-Dobler L, Schmitt HJ, eds. The TBE Book. 7th ed. Singapore: Global Health Press; 2024. doi:10.33442/26613980_13-33-7
References
- Krech, T. [Tick-borne Encephalitis (TBE) in Switzerland] Doctoral thesis, University of Bern. 1980.
- Baumberger P, Krech T, Frauchiger B. [Development of early-summer meningoencephalitis (FSME) in the Thurgau region 1990-1995–a new endemic area?]. Schweiz Med Wochenschr. 1996;126(48):2072-2077.
- Aberham C, Radda A, Holzmann H, Krech T. Detection of tick-borne encephalitis (TBE) virus in Liechtenstein. Zentralbl Bakteriol. 1992;277(4):554-560. doi:10.1016/s0934-8840(11)80481-0
- Schwanda M, Oertli S, Frauchiger B, Krause M. Die Frühsommer-Meningoenzephalitis im Kanton Thurgau: eine klinisch-epidemiologische Analyse [Tick-borne meningoencephalitis in Thurgau Canton: a clinical and epidemiological analysis]. Schweiz Med Wochenschr. 2000;130(41):1447-1455.
- Bundesamt fuer Gesundheit (BAG). [Infectious Disease Reporting – Tick-borne Encephalitis – TBE]. 2023. Accessed 30 March, 2024. https://www.bag.admin.ch/bag/de/home/krankheiten/infektionskrankheiten-bekaempfen/meldesysteme-infektionskrankheiten/meldepflichtige-ik/meldeformulare.html#-1611150545.
- Altpeter E, Zimmermann H, Oberreich J, Péter O, Dvořák C; Swiss Sentinel Surveillance Network. Tick related diseases in Switzerland, 2008 to 2011. Swiss Med Wkly. 2013;143:w13725. Published 2013 Jan 8. doi:10.4414/smw.2013.13725
- Schmidt AJ, Altpeter E, Graf S, Steffen R. Tick-borne encephalitis (TBE) in Switzerland: does the prolongation of vaccine booster intervals result in an increased risk of breakthroughs?. J Travel Med. 2022;29(2):taab158. doi:10.1093/jtm/taab158
- Schuler M, Zimmermann H, Altpeter E, Heininger U. Epidemiology of tick-borne encephalitis in Switzerland, 2005 to 2011. 2014;19(14):pii/20765]. Euro Surveill. doi:10.2807/1560-7917.es2014.19.13.20756
- Euro-Lex. Commission Implementing Decision (EU) 2018/945 of 22 June 2018 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions. Official Journal of the European Union. Accessed 30 March, 2024. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=uriserv%3AOJ.L_.2018.170.01.0001.01.ENG.
- Bundesamt für Gesundheit BAG. [Numbers for Infectious Illnesses – Tick-borne Encephalitis – TBE]. Accessed 30 March, 2024. https://www.bag.admin.ch/bag/de/home/zahlen-und-statistiken/zahlen-zu-unfektionskrankheiten.exturl.html/aHR0cHM6Ly9tZWxkZXN5c3RlbWUuYmFn YXBwcy5jaC9pbmZyZX/BvcnRpbmcvZGF0ZW5kZXRhaWxzL2QvZnNtZS5odG1sP3dlYmdy/YWI9aWdub3Jl.html
- Ackermann-Gäumann R, Eyer C, Vock M, et al. Prevalence of anti-tick-borne encephalitis virus (TBEV) antibodies in Swiss blood donors in 2014-2015. Blood Transfus. 2023;21(2):100-109. doi:10.2450/2022.0099-22
- Lammli, B., Muller, A. & Ballmer, P. E. [Late sequelae of early summer meningoencephalitis]. Schweiz Med Wochenschr 2000;130:909-915.
- Zimmermann, H. & Koch, D. [Epidemiology of tick-borne encephalitis (TBE) in Switzerland 1984 to 2004]. Ther Umsch. 2005;62:719-25. doi:10.1024/0040-5930.62.11.719
- Bundesamt für Gesundheit BAG. [Tick-borne encephalitis (TBE): expansion of risk areas].Accessed 30 March, 2024. https://www.bag.admin.ch/dam/bag/de/dokumente/mt/i-und-b/richtlinien-empfehlungen/empfehlungen-spezifische-erreger-krankheiten/zeckenenzephalitis/zeckenenzephalitis-impfung-risikogebiet.pdf.download.pdf/zeckenenzephalitis-impfung-risikogebiet-de.pdf
- Bundesamt für Gesundheit BAG. [Tick-borne Encephalitis (TBE): continuted increase in reported cases in 2006]. Accessed 30 March, 2024.https://www.bag.admin.ch/dam/bag/de/dokumente/nat-gesundheitspolitik/klimawandel/hitzewelle/hintergrundinfos/info-zecken/zeckenenzephalitis-2006.pdf.download.pdf/zeckenenzephalitis-2006.pdf
- Wicki R, Sauter P, Mettler C, et al. Swiss Army Survey in Switzerland to determine the prevalence of Francisella tularensis, members of the Ehrlichia phagocytophila genogroup, Borrelia burgdorferi sensu lato, and tick-borne encephalitis virus in ticks. Eur J Clin Microbiol Infect Dis. 2000;19(6):427-432. doi:10.1007/s100960000283
- Casati S, Gern L, Piffaretti JC. Diversity of the population of Tick-borne encephalitis virus infecting Ixodes ricinus ticks in an endemic area of central Switzerland (Canton Bern). J Gen Virol. 2006;87(Pt 8):2235-2241. doi:10.1099/vir.0.81783-0
- Gäumann R, Mühlemann K, Strasser M, Beuret CM. High-throughput procedure for tick surveys of tick-borne encephalitis virus and its application in a national surveillance study in Switzerland. Appl Environ Microbiol. 2010;76(13):4241-4249. doi:10.1128/AEM.00391-10
- Burri C, Bastic V, Maeder G, Patalas E, Gern L. Microclimate and the zoonotic cycle of tick-borne encephalitis virus in Switzerland. J Med Entomol. 2011;48(3):615-627. doi:10.1603/me10180
- Lommano E, Burri C, Maeder G, et al. Prevalence and genotyping of tick-borne encephalitis virus in questing Ixodes ricinus ticks in a new endemic area in western Switzerland. J Med Entomol. 2012;49(1):156-164. doi:10.1603/me11044
- Lommano E, Dvořák C, Vallotton L, Jenni L, Gern L. Tick-borne pathogens in ticks collected from breeding and migratory birds in Switzerland. Ticks Tick Borne Dis. 2014;5(6):871-882. doi:10.1016/j.ttbdis.2014.07.001
- Rieille N, Bressanelli S, Freire CC, et al. Prevalence and phylogenetic analysis of tick-borne encephalitis virus (TBEV) in field-collected ticks (Ixodes ricinus) in southern Switzerland. Parasit Vectors. 2014;7:443. Published 2014 Sep 22. doi:10.1186/1756-3305-7-443
- Stegmüller S, Qi W, Torgerson PR, Fraefel C, Kubacki J. Hazard potential of Swiss Ixodes ricinus ticks: Virome composition and presence of selected bacterial and protozoan pathogens. PLoS One. 2023;18(11):e0290942. Published 2023 Nov 13. doi:10.1371/journal.pone.0290942
- Burri C, Korva M, Bastic V, Knap N, Avsic-Zupanc T, Gern L. Serological evidence of tick-borne encephalitis virus infection in rodents captured at four sites in Switzerland. J Med Entomol. 2012;49(2):436-439. doi:10.1603/me11084
- Casati Pagani S, Frigerio Malossa S, Klaus C, et al. First detection of TBE virus in ticks and sero-reactivity in goats in a non-endemic region in the southern part of Switzerland (Canton of Ticino). Ticks Tick Borne Dis. 2019;10(4):868-874. doi:10.1016/j.ttbdis.2019.04.006
- Rieille N, Klaus C, Hoffmann D, Péter O, Voordouw MJ. Goats as sentinel hosts for the detection of tick-borne encephalitis risk areas in the Canton of Valais, Switzerland. BMC Vet Res. 2017;13(1):217. Published 2017 Jul 11. doi:10.1186/s12917-017-1136-y
- Fouché N, Oesch S, Ziegler U, Gerber V. Clinical Presentation and Laboratory Diagnostic Work-Up of a Horse with Tick-Borne Encephalitis in Switzerland. Viruses. 2021;13(8):1474. Published 2021 Jul 28. doi:10.3390/v13081474
- Magouras I, Schoster A, Fouché N, et al. Neurological disease suspected to be caused by tick-borne encephalitis virus infection in 6 horses in Switzerland. J Vet Intern Med. 2022;36(6):2254-2262. doi:10.1111/jvim.16533
- Bundesamt für Gesundheit BAG. Tick-borne Encephalitis (TBE). Accessed 27 March, 2024. https://www.bag.admin.ch/bag/de/home/krankheiten/krankheiten-im-ueberblick/fsme.html
- Bundesamt für Gesundheit BAG. Recommendation for Vaccination against Tick-borneEncephalitis. Accessed 27 March, 2024. https://www.bag.admin.ch/dam/bag/de/dokumente/nat-gesundheitspolitik/klimawandel/hitzewelle/hintergrundinfos/info-zecken/impfempfehlungen.pdf.download.pdf/impfempfehlungen.pdf
- Bundesamt für Gesundheit BAG. Update and new presentation of the map with vaccination recommendation for tick-borne encephalitis as of April 2013. Accessed 27 March, 2024. https://www.bag.admin.ch/dam/bag/de/dokumente/mt/i-und-b/richtlinien-empfehlungen/empfehlungen-spezifische-erreger-krankheiten/zeckenenzephalitis/zeckenenzephalitis-impfung-karte.pdf.download.pdf/zeckenenzephalitis-impfung-karte-de.pdf
- Empfehlungen zur Impfung gegen Frühsommer- Meningoenzephalitis (FSME). Accessed 27 March, 2024. https://www.bag.admin.ch/dam/bag/de/dokumente/mt/i-und-b/richtlinien-empfehlungen/empfehlungen-spezifische-erreger-krankheiten/zeckenenzephalitis/empfehlungen-zur-impfung-gegen-fsmeweb.pdf.download.pdf/240424_Empfehlungen%20zur%20Impfung%20gegen%20FSME_WEB_d.pdf
- Bundesamt für Gesundheit BAG. Swiss Immunization Schedule. Accessed 27 March, 2024. https://www.bag.admin.ch/bag/de/home/gesund-leben/gesundheitsfoerderung-und-praevention/impfungen-prophylaxe/schweizerischer-impfplan.html
- Zens, K. D. et al. A Combined Cross-Sectional Analysis and Case-Control Study Evaluating Tick-Borne Encephalitis Vaccination Coverage, Disease and Vaccine Effectiveness in Children 0-17 in Switzerland, 2005-2022. Euro Surveill 2024;29(18):2300558. doi:10.2807/1560-7917.ES.2024.29.18.2300558
- Baroutsou V, Zens KD, Sinniger P, Fehr J, Lang P. Analysis of Tick-borne Encephalitis vaccination coverage and compliance in adults in Switzerland, 2018. Vaccine. 2020;38(49):7825-7833. doi:10.1016/j.vaccine.2020.10.022
- Compendium.ch. FSME-IMMUN CC Inj Susp. Accessed 27 March, 2024. https://compendium.ch/product/1364944-fsme-immun-cc-inj-susp-sep-nadel.
- Zens KD, Haile SR, Schmidt AJ, et al. Retrospective, matched case-control analysis of tickborne encephalitis vaccine effectiveness by booster interval, Switzerland 2006-2020. BMJ Open 2022;12:e061228. doi:10.1136/bmjopen-2022-061228
- Oechslin CP, Heutschi D, Lenz N, et al. Prevalence of tick-borne pathogens in questing Ixodes ricinus ticks in urban and suburban areas of Switzerland. Parasit Vectors. 2017;10(1):558. Published 2017 Nov 9. doi:10.1186/s13071-017-2500-2
- Berger T, MM, Ackermann-Gäumann R, Moor D, Ingenhoff JE. in Swiss Society for Microbiology. 2023.
- Compendium.ch. [Technical Information]. Accessed 27 March, 2024. https://compendium.ch/product/105785-encepur-n-inj-susp/mpro
- Compendium.ch. [Technical Information]. Accessed 27 March, 2024. https://compendium.ch/product/1364944-fsme-immun-cc-inj-susp-sep-nadel/mpro
- Compendium.ch. [Technical Information]. Accessed 27 March, 2024. https://compendium.ch/product/1269220-fsme-immun-junior-inj-susp-o-na/mpro.
- Bundesamt für Gesundheit BAG.[Cantonal vaccination coverage surveillance Switzerland]. Accessed 27 March, 2024. https://www.bag.admin.ch/bag/de/home/gesund-leben/gesundheitsfoerderung-und-praevention/impfungen-prophylaxe/informationen-fachleute-gesundheitspersonal/durchimpfung.html. 2020.