Anna Mazanik
Key points
- The TBE virus was first isolated in 1937 by the team of Lev Zilber during their expedition to the Soviet Far East (today the Khabarovsk and Primorie regions of Russia). The same expedition also established the connection between the disease and the tick vector.
- After the isolation of the virus, several studies established numerous older cases of TBE in the Soviet Far East, Siberia, and the Urals dating back to the early 1900s. The first retrospectively diagnosed case was identified by Mikhail Chumakov in Tatarstan and dates back to 1895.
- A separate line of Soviet research studied Kozhevnikov epilepsy (epilepsia partialis continua), one of the many possible symptoms of TBE and/or TBE sequelae. In 1922 Vladimir Omorokov examined 27 cases of Kozhevnikov epilepsy from Western Siberia and suggested that the infectious agent was linked to the forest and its insects.
- Although TBE was present in many parts of Russia at the turn of the twentieth century, it became much more visible in the Soviet Far East in the 1930s due to the mass deportations and forced labor in the region, which resulted in higher exposure and severity of disease.
- In 1938-39, Soviet virologists Nadezhda Kagan and Elizaveta Levkovich developed the first vaccine against TBE, which was then tested on the unfree population in the Khabarovsk region.
- Due to the extreme conditions in which that population lived, including severe malnutrition and exploitation, the early Soviet epidemiological data on TBE needs to be used and interpreted with caution.
Introduction
The history of the discovery of TBE in the Soviet Far East and the isolation of the virus is well known in the scientific literature. It has been a subject of a number of publications, both in Russian and in English1-6 including also the earlier editions of the TBE Book.
In the 1930s, an outbreak of a severe paralytic disease was recorded in the southern parts of the Soviet Far East. In 1937, the People’s Commissariat of Public Health, the Soviet equivalent of a public health ministry, organized a scientific expedition, led by Jewish virologist Lev Zilber (Silber), to investigate the reports of the unknown disease in the region of Khabarovsk. Zilber’s expedition established the viral etiology of disease, which soon became known in Russian as “tick-borne encephalitis” (kleshchevoi entsefalit) and in English as “Russian spring-summer encephalitis”; the expedition isolated the causative virus from the patients and the ticks using mouse brain, thus identifying ixodid ticks as its vectors. The subsequent expeditions in 1938-1939 described the circulation of the virus, vector species and reservoir hosts. Largely on the basis of that research, parasitologist Evgeny Pavlovsky developed his famous natural nidality theory of transmissible disease, which applied the ecological niche approach to the study of zoonoses and soon became the key to studies of the environmental circulation of arthropod-borne viruses.
That early Soviet research on TBE in the 1930s and 1940s has been crucial for the understanding of TBE, its etiology, clinical picture, and epidemiology until the present day, both in Russia and internationally. However, some of this early research has in fact been misrepresented in the scientific literature and obscured by Soviet censorship. In the current chapter, based on the analysis of previously unstudied historical documents, I would like not only to retell the key steps of that familiar story, but to discuss how those early expeditions fit into the broader Soviet scientific, environmental, and socio-political context and what it means for the interpretation of Soviet TBE research and the history of TBE.
Considering the wide spread of TBE across Eurasia and Russia, it is remarkable that TBE – supposedly – captured scholarly attention only in the 1930s. The first subchapter here analyzes the history of TBE “before the TBE virus”, that is before 1937, and puts together scientific records on the localization and understanding of this disease before it received its name and before its etiology became known. The second subchapter asks why, then, this disease became particularly visible in the 1930s and why specifically in the Soviet Far East. Looking at the social, environmental, and political developments in the region, it shows the “emergence” of this disease was inseparable from the geopolitical agendas and the Stalinist colonization of the Far Eastern peripheries through involuntary resettlement and forced labor. Finally, the last subchapter looks at how this influenced early Soviet studies of TBE and the interpretation of their findings.
TBE “before the TBE virus“
The story of TBE in the Soviet Union typically begins in the early 1930s. Since 1932 physicians in the Soviet Far East observed clusters of cases of a severe infection with a high case-fatality rate. Depending on the symptoms, it was described as poliomyelitis, meningitis, or “toxic influenza”. In 1935 Vladivostok-based navy neurologist A.G. Panov recognized this disease as infectious encephalitis and noted its distinct spring-summer seasonality.7 This opened the way for a suggestion that the disease might in fact be a form of Japanese encephalitis, for which the causative agent had been identified in Japan shortly before that—the misconception that spread beyond scientific circles and, as I will show later in the chapter, played a tragic role in the careers of early TBE researchers. In 1936 the Khabarovsk regional department of public health created a special medical unit of local neurologists and physicians led by Israel Finkel to carry out the studies of this disease, but its exact etiology remained unknown. Finkel also authored the first publication on “Far Eastern encephalitis” in a local medical journal. There were some attempts to isolate viruses from the brain of those succumbed to the disease, but the strain was quickly lost, and the causative link could not be proven.3,8,9 Although these early studies in themselves contained no major scientific breakthroughs, they helped accumulate important epidemiological and clinical evidence to suggest that the disease was likely viral and vector-borne. This evidence provided a starting point for Zilber’s scientific mission in 1937 and contributed to its quick success.
The observed disease clusters of the 1930s were, however, not the earliest cases of probable TBE. Already the first expeditions tried to find earlier cases through checking the hospital records and patients’ histories and examining the local population in search of the long-term symptoms of the past disease. N. Dankovskii and A. Drobyshevskaia identified two local cases of TBE from the early 1920s with residual paresis of the extremities that was still visible seventeen years later. Serum of the survivors protected mice from a challenge with TBEV-preparations from mouse brain.10,11 Panov mentions reports of local physicians suggesting that cases of a disease similar to TBE had been observed in 1920 among the partisans hiding in the Far Eastern taiga during the Russian Civil War.7
The earliest retrospectively identified cases of TBE in the Far East were later reported by Aleksei Shapoval, a local neurologist who had been involved in the Khabarovsk medical group on TBE in 1936, in Zilber’s expedition, and in many subsequent investigations of this disease in the region. He described several patients from the regions of Khabarovsk and Primorie with residual symptoms of possible TBE, which had started after a severe febrile illness during the summer months, one from 1909, examined in 1937, another one from 1917, examined in 1941, and the third one from 1911, examined in 1949. Additionally, Shapoval also mentioned a possible cluster of TBE in 1904 in a forestry near Nikolaievsk-on-Amur with 17 cases and 3 deaths with symptoms of fever, headaches, vomiting, blurred consciousness, and paralysis. One of the survivors of this outbreak was examined in 1939 by S. Vaflin (so not by Shapoval himself) and was found to have paresis of the upper extremities. If we accept this indirect evidence, this 1904 outbreak can be considered to be the earliest known historical cluster of possible TBE cases in the Russian Far East – and also the biggest before the Soviet period.12
Importantly, the Far East was not the only location of the early TBE reports in Russia. Cases of a very similar disease had already caught the attention of physicians in other parts of the country, in particular, in the Urals and Western Siberia, but had been described under different names, for example, as atypical poliomyelitis.6,13 A.A. Pecherkin (Perm), M.G. Polykovskii (Sverdlovsk / Yekaterinburg) and N.V. Shubin (Tomsk) had sent reports about this disease to the All-Union Institute of Experimental Medicine, but it was not until early 1939 that they, together with the serum samples from recovered patients, were tested by Moscow virologists and the link to TBE was confirmed by using the serum of survivors in a TBEV-mouse-challenge test. As a result, a special expedition was sent to the regions of Sverdlovsk and Perm to investigate the presence of TBE there. This expedition was led by Mikhail Chumakov, a talented virologist who had survived and had been left permanently disabled by a TBE infection he had contracted during Zilber’s expedition in 1937 by conducting the autopsy on a patient who had died from TBE. Through retrospective diagnosis, confirmed by serological studies, Chumakov and Zeitlenok managed to identify several possible past TBE cases in the Urals, the earliest of which went back to 1914.14 Ten years later, however, Mikhail Chumakov managed retrospectively to identify an even earlier case. In 1949, Chumakov, by then a very established virologist, was sent to investigate a TBE outbreak in the Tatar ASSR (today the Republic of Tatarstan in Russia). There he found a 72-year old man from the village of Urgancha (about 200 km east of Kazan) with post-encephalitis symptoms, who had fallen ill in May 1895, diagnosed by Chumakov as TBE. He emphasized the “historical importance” of this case and described it in his report to the Russian (RSFSR) Ministry of Public Health, preserved in the ministry’s archival fonds.15 This may be the earliest historical (retrospectively) clinically diagnosed case of tick-borne encephalitis.
Of separate importance for reconstructing the history of TBE in Russia is the question of the relation between TBE and Kozhevnikov epilepsy. Kozhevnikov epilepsy (epilepsiea partialis continua), first described by Russian neurologist Aleksei Kozhevnikov in 1894, is a syndrome with many possible causes.16 One of these causes is TBEV infection, and this causality is common in the Eastern parts of Russia.17 In 1922 L.I. Omorokov, a professor from Tomsk in Western Siberia, published a study of 27 cases of Kozhevnikov epilepsy observed over three years. Based on his cases, Omorokov described Kozhevnikov epilepsy as a syndrome of encephalitis, caused by an infectious agent. Even more importantly, he suggested the link between this disease and the taiga and its insects:
“What is striking is the fact that all the sick are peasants, manual workers, living mostly in the taiga, who were born in the Tomsk, Tobolsk, Altai and Yenisei gubernia. This fact in our opinion can shed some light on the etiology of this suffering that is so rare in Europe and in European Russia and is so frequent in Siberia […] In our large material there has not been a single case from the intellectual classes. Therefore we need to recognize that Kozhevnikov epilepsy is tightly linked to the peasant population of the Siberian taiga. Perhaps the climatic conditions, the harshness of the climate, the difficult conditions of living in the taiga as well as the abundance of insects, that is mosquitos and flies, is one of the preconditions of the appearance of this form of encephalitis.” 18
In 1939 it was recognized that the cases studied by Omorokov had possibly been cases of TBE based on clinical descriptions and the epidemiological situation. Omorokov’s 1922 article can be considered the first description of that specific manifestation of TBE and the first suggestion of its link to the forest and the possibility of the vector-borne etiology.19 In some of the cases observed by Omorokov the onset of the symptoms started long before the examination, with the earliest case from 16 years before, that is from the 1900s, and at least six cases dating back to the 1910s. The majority of the cases, however, were very recent or new, from 1917-1922, the period of the Russian revolution and Civil War, a time of extreme hardship, violence, displacement and severe food scarcity as well as radical food expropriations from the peasants by the new Soviet authorities. It is possible that this time of crisis contributed to a certain emergence of TBE in the region, as the local population intensified their contact with the forest (as a place to hide or to search for food) while malnutrition could have increased the severity of disease.
What all this evidence suggests is that there clearly had been sporadic cases of TBE in the Far East, the Urals, Western Siberia and Tatarstan going back to the 1890s-1920s. Although those cases were rare, they were often severe and noticeable enough to attract the attention of local physicians and scientists who presented their materials in published papers and reports to their superiors, even if they described this disease as Kozhevnikov epilepsy or atypical poliomyelitis, but these reports did not result in further investigation. What, then, made the outbreak in the Soviet Far East in the 1930s so distinct to ensure that a special expedition with considerable resources, equipment, and experts from the top research institutions in Moscow and Leningrad went there?
The emergence of TBE in the Soviet Far East: Environmental, social, and political factors
Early Soviet research on TBE often described Far Eastern taiga as virgin, as a kind of “untouched” nature, tabula rasa unaffected by humans, which was to be transformed, cultured and “healthified” under socialism. Such bias was quite typical of many modern European scientists in colonial spaces, who often failed to grasp the complexities of human-environment interaction in local and indigenous communities but was exacerbated by the Soviet tendency to downplay pre-revolutionary developments. In fact, the region that became the space of the early TBE research experienced dramatic socio-environmental transformation in the late imperial period. It was annexed by the Russian Empire in 1858-1860 and at that moment was sparsely populated by Indigenous hunter-gatherer communities. In the following half a century it experienced dramatic population growth because of the arrival of Russian, Ukrainian, and Korean settlers, re-emergence of settled agriculture (that had ceased to exist for several hundred years following the destruction of medieval settlements by the Mongol invasion), deforestation (due to clearing, the construction of infrastructure, wood-logging, erosion, and mass forest fires) as well as widely reported overhunting of predators. Throughout the 1920s and 1930s these processes were supplemented by the early conservation policies, the creation of nature reserves and the establishment of deer farms to harvest deer antlers (which were considered a precious export commodity because of their value in Chinese medicine).20 These processes are not only of historical but also of biological importance as they could have affected animal migration, the population of vectors and their hosts and the circulation of the virus.
Clearly, imperial colonizers—peasants, Cossacks, scientists, explorers, forestry workers— had to come into frequent contact with the taiga. Furthermore, late imperial accounts often mention the abundance of ticks in Far Eastern forests and report frequent tick bites, usually multiple at the same time.21,22 So there had clearly been humans in the Far Eastern taiga before the 1930s and they had frequently been bitten by ticks, yet there seems to have been only sporadic cases of TBE. Later studies also specifically looked for the cases compatible with a TBEV infection among the Indigenous Orochen and Udeghe peoples in the region, whose life had been directly tied to the forest, but failed to identify more than a couple of cases.12
The situation changed radically in the Stalinist period when suddenly TBE cases in the region started to appear in dozens. Not only did the colonization and industrial development of the region intensify, but it relied strongly on involuntary and semi-voluntary resettlement and forced labor. By the end of the 1930s, about 20% of the population of the entire Far Eastern region were unfree, and it was these groups that were used in the heavy labor in wood-logging, mines, and infrastructure construction.23, 24 Due to its remote location and the shortcomings of Soviet central planning and distribution system, throughout the 1930s this region remained constantly undersupplied. The scarcity of food and clothes was known even to the privileged groups, such as the military and the free administrative personnel,25 but the conditions of prisoners and deported special settlers in the GULAG (Glavnoie upravleniie ispravitel’no-trudovykh lagerei) system of camps and special settlements were simply horrendous, characterized by extreme undernutrition, vitamin deficiencies, lack of basic supplies, exhaustive labor and constant stress connected to the arrest, deportations, and imprisonment. There exists considerable scholarship on the influence of social factors on the TBE morbidity as well as on the relations between malnutrition and viral infections, that show that malnutrition, low calorie intake and vitamin deficiencies weaken the immune system and increase the risk of severe course and complications and death.26-29 All of these factors were present in the GULAG camps and settlements and to some extent also influenced other forms of organized labor (military units, Komsomol brigades, worker parties), which also depended on the very poor centralized supply system. Furthermore, many of the newcomers of the Stalinist period came from the steppe regions and had likely not been previously exposed to the TBEV. The morbidity among newcomers was much higher than that of earlier (for example, Korean) settlers in the same location. 12
Another important factor in the apparent emergence of TBE in the Far East, or rather its perception, was geopolitical. At that time this remote Russian periphery was gaining strategic importance following the occupation of Manchuria by Japan in 1931. The repeated border clashes and the fear of a Japanese attack forced Soviet leadership to station considerable military and industrial forces along the border with Manchuria. It was the Red Army that requested the special expedition to study encephalitis in the Far East.3 Apart from the general concern about the potential spread of disease among the military personnel, the possible connection of the new disease to Japanese encephalitis led to a fear that the outbreaks could have been a result of the Japanese attack. This view was shared by the highest ranks of the Soviet military and was in fact not as bizarre as it might sound today, considering the existence of the strong bioweapon program in Japan at the time. It was therefore the military concerns that ensured that the disease outbreaks in the Far East would not go unnoticed as those in the Urals and Western Siberia but that a special expert mission from the center, located 7,000 km away, would be sent there and would eventually succeed in identifying the virus.
The implications for early Soviet TBE research
When commissioned with the tasks to lead an expedition to the Far East, Zilber managed to bring together an interdisciplinary team of virologists, entomologists, epidemiologists and clinicians. Importantly, about half of the members of Zilber’s expedition were women, including both deputy heads, virologists Elizaveta Levkovich and Alexandra Sheboldaeva. The mission arrived at Khabarovsk in mid-May 1937 and was divided into two units. The southern unit was located in Vladivostok at the local microbiological laboratory and the northern in the village of Obor. It is worth having a closer look at it, as much of the early research was shaped by disease ecologies of this specific location.
Obor is located on the banks of the river with the same name southeast of Khabarovsk (ca. 100 km away by road today). The development of this area started at the turn of the 1930s with the construction of the Obor railway and the Obor forestry industrial complex. Its population had a very distinct composition, as it consisted primarily of deported special settlers, distributed across several camps belonging to the forestry. The first large cohort of special settlers—7,400 persons deported from the south of European Russia and the Volga region—was brought there in 1931.10,30 In addition to the deportees, the Obor forestry complex also used the labor of prisoners–the GULAG report of 1933 sets the quota of 800 prisoners to be sent to the area.31 The conditions in the Obor forestry were typical for the GULAG structures with their extreme undernutrition, exploitation and abuse, and in the first half of the 1930s perhaps even worse than average in that outstandingly brutal and inhumane system. For example, a 1932 security service report states that “the food situation was particularly acute in the Obor and Tygda districts of special settlements where the shortages of supplies resulted in a true famine.”32 Food scarcity remained severe in the following years. Undernutrition must have significantly affected the interaction of human bodies with the virus and could have disadvantaged the new migrants to the Far East vis-à-vis the colonizers of the late imperial period, contributing to the rise in the numbers and severity of symptomatic TBE infections. There were other factors that undermined the health status of the residents of Obor and could have influenced the ways their bodies responded to the virus when infected—exploitative physical labor in wood-logging with low mechanization, hypothermia because of the constant work outside in a wet, swampy area, lack of warm clothes and footwear and inadequate housing, various comorbidities that were common in the conditions of overcrowding, lack of sanitation and very poor healthcare, extreme stress connected to the traumatic experiences of deportation, arrest, family separation and adaptation to the camp environment, as well as direct torture and abuse.
In addition, the residents of Obor had a significantly increased exposure risk. They spent long working hours in the taiga thickets because of the nature of their labor with minimal precautions of occupational health. Furthermore, in the situation of dramatic undersupply of food, the forest was not only a place of their hard labor but also their main ally in the fight against starvation and scurvy. The camp administration encouraged foraging as the berries, mushrooms, and herbs could compensate for the lack of provisions evident from official reports.33 The other dimension was the lack of any protection against exposure to tick-bites, and this too could have distinguished settlers of the Stalinist times from the earlier colonizers and the Indigenous people who lived in the area. Even today the key protection against tick-borne disease, apart from vaccination, is adequate clothing and footwear, and regular inspection of the body to remove ticks before they bite. All of these were unavailable to the special settlers and prisoners in Obor. First of all, the wear and tear of cloths was intense in the thickets of the Far Eastern taiga. New – or any other – clothes were, however, virtually impossible to procure. The lack of clothes and footwear was a constant refrain of the official reports of the time, which affected not only prisoners and special settlers but also peasants, soldiers, and the camp administration. Furthermore, the inspection of the body and the early detection of ticks was also extremely complicated among the exhausted workers living in the poorly heated and lit overcrowded barracks.
Medical research in the GULAG has recently come to the attention of historians, who revealed the “conspicuous silence” of Soviet scientists, many of whom were also prisoners, about the social context of their research subjects, when any references to camps, starvation and ruthless exploitation were avoided.34-36 Clearly, these conditions could not have evaded either the local medical researchers in the Far East, or the members of the Zilber’s expedition but due to political reasons they could only hint at the social status of the Obor residents in their early publications, for example, by referring to the local population as a “contingent” that “was brought” rather than “came” to the area and describing their working and living conditions as “difficult” or “unsatisfactory”. The TBE morbidity and fatalities that they recorded in the Obor forestry were remarkable, with 60-80 symptomatic cases per season and 15-20 deaths (see Table 1). There is no exact data on the severity of disease and the complications, but the expedition’s epidemiological study mentions that out of 8 confirmed cases of TBE in 1933, 6 survivors remained severely disabled which suggests that post-infection disability was very frequent.37
Table 1: TBE cases and fatality rates in the Obor forestry industrial complex.37
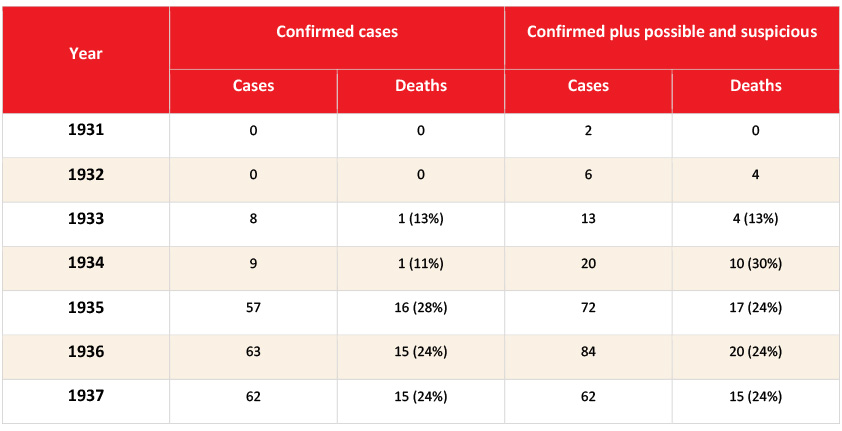
Click the image above to enlarge
“Confirmed cases”: neurological residual symptoms after infectious encephalitis; “possible cases”: infectious encephalitis without a neurological examination or no residual symptoms observed; “suspicious cases”: death at a young age with a diagnosis labeled as “meningitis”, “paralysis”, “paresis” or “intracerebral hemorrhage”.
Zilber’s expedition lasted for three months, and in this short period it identified a new distinct form of viral encephalitis and isolated 29 strains of the causing virus, described the tick vector, the epidemiology and pathophysiology of disease and its clinical manifestation and showed some efficiency of serotherapy against it. Although Zilber’s success is usually told as an exclusively Soviet story, it of course did not happen in isolation from the international science. Zilber and his colleagues read and widely cited foreign research on encephalitis, particularly American and Japanese. Even more importantly, there was also a transborder exchange of viral strains. Already during the expedition, in summer 1937 Zilber asked for and received a Kalinin strain of the Japanese encephalitis virus from Japan, through the Soviet Embassy in Tokyo – quite remarkable given the political and military tensions between the two countries. The strain of the St. Louis encephalitis virus was received from L.T. Webster in New York. These strains were immediately used in the expedition research and helped confirm the distinctiveness of the TBE virus.3,10
Such international cooperation had tragic consequences for Zilber and some of his colleagues. At the height of the Stalinist purges it seemed to be more fitting for the Soviet security authorities and military leadership to view the disease outbreaks in the Far East as cases of Japanese encephalitis and therefore not as a result of their mismanagement but as an act of sabotage and Japanese attack. Upon his return to Moscow, Zilber was arrested on the accusation of being a Japanese spy and intentionally spreading Japanese encephalitis among the Soviet population. Two of his female colleagues–Alexandra Sheboldaeva and Tamara Safronova–were arrested because of their connection to Zilber. Israel Finkel was also arrested and most likely perished in prison.3 Zilber was soon released and managed to take part in the all-union conference of microbiologists in January 1939 and since then the distinctiveness of tick-borne encephalitis was recognized in Soviet publications. However, in 1940 he was arrested again and released only in 1944, following the intervention of several prominent virologists and his former partner, Soviet penicillin researcher Zinaida Ermolieva.38 The research on the virus and the expeditions to the Far East continued without Zilber, but it is clear that his arrest must have made Soviet scientists even more cautious.
Given the high case fatality and disability rates, including among the Soviet scientists themselves, the prevention of disease immediately became a priority of research. Work on the vaccine started in 1938 and was led by two female virologists, both affiliated with Moscow’s All-Union Institute of Experimental Medicine: Nadezhda Kagan in Moscow and Elizaveta Levkovich, who had been a deputy head of Zilber’s expedition, in the field in the Khabarovsk region. The laboratory where the research was conducted was also staffed with female personnel. In the autumn of 1938 Kagan contracted TBEV after exposure in the laboratory and died, and Levkovich took over her work. Two months later, a laboratory technician Natalia Utkina also died after contracting TBE. Women’s bodies were also the first to try the new vaccine, based on the Sofyin strain, when Levkovich and her assistant Galina Zorina-Nikolaieva tested the vaccine on each other in 1939.3, 39, 40
To check the efficiency of the vaccine, the 1939 expedition conducted trials, designed as a kind of unblinded cluster-randomized trials, on the population of the endemic area in Obor. The 1941 publication of the results speaks of 925 vaccinated subjects and a control group of 1,185 unvaccinated subjects that were distributed across four locations within the Obor forestry-industrial complex and had a comparable age, gender and occupational composition. This account does not mention the legal status of the participants but says that both groups were offered “sanitary explanation” about the trials although it is unclear what exactly that explanation implied. It was not until 2001 that the memoir of the neurologist Aleksei Shapoval, involved in those trials, revealed the circumstances in which they were conducted. Shapoval speaks of 1,987 vaccinated subjects and explicitly states that they were inmates of a forced labor camp while another camp with 2,387 prisoners in the same area was used as a control group. Such composition of participants would suggest that the involvement in the trial was not voluntary. Luckily for those vaccinated, both accounts agree that the vaccine seemed to be successful and offered some protection against the disease (the official publication reported only 2 mild TBE cases among the vaccinated compared to 27 cases and 7 deaths among the control group; Shapoval recalls 9 mild TBE cases among the vaccinated compared to 37 TBE cases and 12 deaths in the control group).39,40,41 The case-fatality rate of TBE observed in the early trials (27-32% in the unvaccinated group) was dramatic. These most likely involuntary vaccine trials on the unfree population did not contradict the scientists’ compassion and probably sincere desire to protect that population from a potentially deadly disease -after the arrest of Zilber and his colleagues, the expedition members knew very well that they could easily end up in a similar camp themselves. Yet, again, the concealment of the camp context had not only ethical but also empirical implications. The health status and post-infection survival chances of forced laborers or settlers had been severely compromised by very poor nutrition, exhaustive work, the lack of adequate healthcare, and extreme stress connected to deportation and imprisonment. However, Soviet scientists did not reflect on how those factors could have influenced the striking TBE mortality and morbidity they observed and in their publications attributed them exclusively to the properties of the virus, reinforcing the image of tick-borne encephalitis, especially in its Far Eastern manifestation, as highly lethal.
Of all the Soviet scientists involved in the early TBE research, Aleksei Shapoval deserves credit for consistently trying, if not to reveal, then to hint at the social conditions in which TBE emerged to the extent Soviet censorship allowed. Lev Goldfarb, who later worked with Shapoval, mentioned that Shapoval had been deeply affected by Zilber’s arrest,42 perhaps this was one of the reasons why he did not let this important aspect fall into oblivion. In 1947, Shapoval coordinated the treatment of the TBE patients in the Khabarovsk region and it becomes clear from his report to the Public Health Ministry that most of the patients were Japanese prisoners-of-war.43 The forced labor of prisoners-of-war was widely used in the Soviet Far East, and their conditions were comparable to those of other prisoners and special settlers, with undernutrition as a crucial factor affecting their health status and mortality. In Primorie, another Far Eastern region, the situation was very similar – in 1948 the majority of 240 recorded TBE cases occurred among the Japanese prisoners-of-war (the method of TBEV diagnosis is not specified in the source).44 These were unpublished internal reports, but after Stalin’s death with the certain liberalization of the Soviet regime some of this information made it into scientific publications.
In 1961, Shapoval published a monograph entitled “Tick-borne Encephalitis”, in which he questioned the assumption that the changes in the TBE morbidity in the Far East were connected exclusively to the frequency of the contacts with the forest and argued, although with careful phrasing, that the severity of disease depended on the living conditions of the human population. Comparing TBE outcomes across several locations in the Khabarovsk region in 1947, he showed that in settlements with good living conditions and decent food supply the lethality was 8%, in Obor, where the situation had somewhat stabilized by the late 1940s, it was 20%, while in the Amgun unit, where there were “problems with food supply” (probably a euphemism for extreme undernutrition) and where “workers had to build housing for themselves” away from any settlements, the disease was particularly severe and the case fatality was as high as 56%.12 What Shapoval described here was most likely the GULAG Amgun labor camp which used the forced labor of Soviet prisoners and Japanese prisoners-of-war. He also specifically mentioned that the disease was particularly severe among the workers with hunger dystrophy. Admitting that in the socialist state there had been workers with hunger dystrophy was in itself very daring, and this was the kind of diagnosis that for his contemporaries must have signaled that he was describing the workers in the camps. It took, however, forty more years until Shapoval was able to speak about it openly in his memoirs.
Conclusion
The year 1937 and the work of the early Soviet Far Eastern expeditions should always have a very special place in the history of TBE. This is when the virus was first isolated in the mouse brain and the disease etiology was understood and described. It also has to be emphasized that scientists, many of whom were women, worked on this disease at a significant risk for themselves, both medical and political, and although this research propelled the career of some, others had to pay a very high price with their life, health or freedom.
Yet, it is clear that not only the biological but also the documented social history of TBE is longer and broader. Cases of this disease have been recorded in Russian/Soviet territory at least since the 1890s and they occurred both in the Asian and the European parts of the country. In the 1920s and 1930s TBE started capturing the attention of scientists and physicians in various locations, not only in the Far East, but did this under different names such as atypical poliomyelitis or Kozhevnikov epilepsy. This increased attention was linked to the transnational developments in medical sciences and general interest in neuroinfections following the epidemic of the Encephalitis lethargica (Economo encephalitis)—a mysterious infectious brain disease that swept the world in the 1910s and 1920s. It is possible, however, that there was some real increase in the number and severity of TBE cases across the Soviet Union in this time due to the changing patterns of human interaction with the environment and the virus, connected to the hardship and food scarcity during the times of the Civil War, military communism, and collectivization.
The well-known emergence of TBE in the Far East in the 1930s, that eventually led to the isolation of the virus, happened in very special circumstances of Stalinist colonization of the region. That socio-political context dramatically affected the composition, the health status and exposure of the population that lived in or was brought to the region, often by force, and must have influenced the TBE epidemiology, including the severity, clinical manifestations, and lethality of disease. These social circumstances, including extreme undernutrition and exploitative forced labor in the forest without any protection, were a long-lasting reality that continued to affect local disease epidemiology at least until the turn of the 1950s, if not later.
It is important to acknowledge this social context when reconstructing the history of tick-borne encephalitis. One aspect here is ethical, that is the need to, at least in this form, commemorate the many people in the inhumane circumstances who were exposed to this infection and deprived of all the means to resist it. But there can also be empirical implications for scientific research. Since the living conditions of the European and Russian population today–and in fact of the late-Soviet population as well–were and have been, thankfully, very different from that of the Stalinist period, early Soviet epidemiological studies have to be interpreted and used for comparison with caution. These differences in the social context, health status and exposure need to be considered in the long-term and cross-regional TBE epidemiology, especially its Far Eastern variant, as well as the historical evaluation of preventive strategies. At the same time, this new interpretation of early Soviet research could provide important historical precedents for the studies on the role of the social factors in the TBE emergence in the 1990s and could inform future investigations.27,28,45
Acknowledgments
The author would like to thank Anastasia Fedotova for her help in getting access to the 1939 issue of the journal Arkhiv biologicheskikh nauk.
Contact
Anna Mazanik
anna.mazanik@mws-osteuropa.org
Author
Citation
Mazanik A. Early TBE Research in the Soviet Union: revisiting the narrative. Chapter 3a. In: Dobler G, Erber W, Bröker M, Chitimia-Dobler L, Schmitt HJ, eds. The TBE Book. 7th ed. Singapore: Global Health Press; 2024. doi:10.33442/26613980_3a-7
References
- Kisselev LL, Abelev GI, Kisseljov F. Lev Zilber, the personality and the scientist. Adv Cancer Res. 1992;59:1-40. doi:10.1016/s0065-230x(08)60301-2
- Kiselev LL, Levina ES. [Lev Aleksandrovich Zilber, 1894-1966: Life in science]. Moscow: Nauka; 2005.
- Levina ES. [The first virologists and medical virology in the USSR of the 1930s]. Istoriko-biologicheskie issledovaniia. 2010;2(1):10-50.
- Pogodina VV, Karan LS, Levina LS, Kolyasnikova NM, Gerasimov SG, Malenko GV. [75th anniversary of the discovery of tick-borne encephalitis virus. Comparison of early (1937-1945) and modern strains]. Voprosy virusologii. 2012;(S1):66-75.
- Zlobin VI, Pogodina VV, Kahl O. A brief history of the discovery of tick-borne encephalitis virus in the late 1930s (based on reminiscences of members of the expeditions, their colleagues, and relatives). Ticks and Tick-borne Dis. 2017; 8 (6):813-820; doi:10.1016/j.ttbdis.2017.05.001.
- Dobler G, Gniel D. A History of Tick-Borne Encephalitis and Its Virus. In: Vasilakis N, Kramer LD, eds. History of Arbovirology: Memories from the Field. Springer; 2023. doi: 10.1007/978-3-031-22003-6_21
- Panov AG. [Seasonal summer encephalitis]. Vladivostok; 1940.
- Finkel IZ. [About the particularities of the course of encephalitis]. Dal’nevostochnyĭ meditsinskiĭ zhurnal. 1936;(3):30-39.
- Walker L. Public health in the Soviet periphery: The case of tick-borne encephalitis (TBE). NCEEER Working Paper. 2011.
- Zilber LA. [Spring (spring-summer) endemic tick-borne encephalitis]. Arkhiv biologicheskikh nauk.1939;56(2):9-37.
- Dankovskii NL. [Epidemiological characteristics of the spring-summer (taiga) encephalitis]. Arkhiv biologicheskikh nauk. 1939;56(2):176-184.
- Shapoval AN. [Tick-borne encephalitis]. Leningrad: Medgiz; 1961.
- State Archive of the Russian Federation. Stenogram of the scientific conference of the All-Union Institute of Experimental Medicine and the Society of Neurologists and Psychiatrists on the problem of encephalitis, 22 December 1938. 6742:1:104:82.
- Chumakov MP and Zeitlenok NA. [Tick-borne spring-summer encephalitis in the Ural region]. Arkhiv biologicheskikh nauk. 1939;56(2):112-120.
- Report of Prof. M.P. Chumakov and laboratory assistant L.N. Shmelkova about the RSFSR Ministry of Public Health expedition to the Tatar ASSR in July 1949. State Archive of the Russian Federation. 482:49:334:72.
- Kozhevnikov A Ia. [A special type of cortical epilepsy]. Meditsinskoe obozrenie 1894; 12 (14):97-118.
- Mukhin KY, Mameniškienė R, Mironov MB, et al. Epilepsia partialis continua in tick-borne Russian spring-summer encephalitis. Acta Neurol Scand. 2012;125(5):345-352.
- Omorokov LI. Epilepsia partialis continua Kozhevnikova. Sibirskii meditsinskii zhurnal. 1922;1-2:8-18.
- Propper-Grashchenkov NI. [Clinical and histopathological characteristic of seasonal viral encephalitis and Kozhevnikov epilepsy as their variant]. Tezisy dokladov. Moscow: s.n.; 1941.
- Sokolsky M. Taming Tiger Country: Colonization and the Environment in the Russian Far East, 1860-1940. PhD dissertation, Ohio State University; 2016.
- Przhevalskii N. [A travel in the Ussuri land]. Moscow. 1937(1870).
- Arseniev VK. [In the Ussuri Land (Dersu Uzala)]. Vladivostok: Ekho; 1921:71.
- Chernolutskaia EN. [Forced migration in the Soviet Far East in the 1920s-1950s]. Vladivostok: Dal’nauka; 2011.
- Kuzmina MA.[The use of forced labor of prisoners at the great Stalin’s construction projects on the lower Amur, 1929-1955]. Dissertation in History. Komsomolsk-on-Amur; 2004.
- Dudar LA. [Commercial and exemplary trade in the Soviet Far East in the 1930s and 1940s]. In: Chernolutskaia EN ed. Sovetskii Dalnii Vostok v stalinkuiu i post-stalinskuiu epokhu. Vladivostok: IHAE FEB RAS, 2014:46-51.
- Randolph S. Tick-borne encephalitis incidence in Central and Eastern Europe: consequences of political transition. Microbes Infect. 2008;10(3):209-216. 2008;10(3):209-216. doi:10.1016/j.micinf.2007.12.005
- Sumilo D, et al. Socio-economic factors in the differential upsurge of tick-borne encephalitis in Central and Eastern Europe. Rev Med Virol. 2008;18(2):81-95. doi:10.1002/rmv.566
- Godfrey E, Randolph S. Economic downturn results in tick-borne disease upsurge. Parasit Vectors. 2011;4(1):35. doi:10.1186/1756-3305-4-35
- Singh P, Bhatt GC, Singh V, et al. Influence of malnutrition on adverse outcome in children with confirmed or probable viral encephalitis: a prospective observational study. BioMed Res Int. 2015;2015:407473. doi:10.1155/2015/407473
- Kochegarova ED. [With the old methods: The formation of the labor resources in the Far Eastern gold industry in the 1920s and 1930s]. Rossiia I ATR. 2002, 4:11-20, 17.
- Berman MD, Berenzon LI, Kogan LI. to Deputy Chairmen of the OGPU G.G. Yagoda and G.E. Prokofiev on the improvement of the use of prisoners in camps for production. May 17, 1933. Central Archive of the Federal Security Service of the Russian Federation. 2:11:546:20-25. Accessed 21 April, 2024. https://docs.historyrussia.org/ru/nodes/48419#mode/inspect/page/3/zoom/4
- Special report of the Special Department of the OGPU on the political attitudes and counter-revolutionary activities of special settlers, as of October 25, 1932. November 1, 1932. Central Archive of the Federal Security Service of the Russian Federation, 2:10:514:208-228. Accessed 21 April, 2024. http://docs.historyrussia.org/ru/nodes/88496#mode/inspect/page/8/zoom/4
- GULAG Directive No. 674514 to the chief sanitary Officers of corrective labor camps on strengthening the fight against scurvy in the camps. November 2, 1933. State Archive of the Russian Federation, P-9414:1:2741:54-55. Accessed 21 April, 2024. http://docs.historyrussia.org/ru/nodes/50153#mode/inspect/page/3/zoom/4
- Alexopoulos G. Medical research in Stalin’s Gulag. Bull Hist Med. 2016;90(3):363-393. doi:10.1353/bhm.2016.0070
- Healey D. Lives in the balance: Weak and disabled prisoners and the biopolitics of the Gulag. Kritika: Explorations in Russian and Eurasian History. 2015;16(3):527-556.
- Nakhapetov BA. [On the history of the health service of the gulag]. Vopr Istor. 2001;(6):126-136.
- Olshevskaya VL. [Spring-summer encephalitis in an industrial forestry complex]. Arkhiv biologicheskikh nauk. 1939;56(2):164-175.
- Letter from leading medical researchers to I.V. Stalin requesting the release of Professor L.A. Zilber. March 1944. Archive of the President of the Russian Federation, 3:58:255:187-191. Accessed 21 April, 2024. https://docs.historyrussia.org/ru/nodes/330508
- Pogodina VV, ed. [Memoirs about Elizaveta Nikolaievna Levkovich]. Chumakova; 2001.
- Mazanik A. Arbovirology and Cold War collaborations: a transnational history of the tick-borne encephalitis vaccine, 1930-1980. J Hist Med Allied Sci. 2023. doi:10.1093/jhmas/jrad054
- Smorodintseff AA, Kagan NW, Levkovitsch EN, et al. Experimenteller und epidemiologischer Beitrag zur aktiven Immunisierung gegen die Frühling-Sommer-Zeckenencephalitis. Archiv f Virusforsch. 1941;2:1–25. doi:10.1007/BF01240711
- Lev Goldfarb, personal communication, 09.05.2023.
- Shapoval AN. Report on Tick-Borne Encephalitis in the Khabarovsk Region, 1947. State Archive of the Russian Federation, А482:47:7997:10.
- Kravchenko A, Soloviev V. Secret note to the USSR Public Health Minister E. Smirnov on the liquidation of tick-borne encephalitis. 1949. State Archive of the Russian Federation, 8009(secret part):32:668:9-13.
- Zavadska D, Odzelevica Z, Karelis G, et al. Tick-borne encephalitis: A 43-year summary of epidemiological and clinical data from Latvia (1973 to 2016). PLoS ONE. 2018. 13(11): e0204844. https://doi.org/10.1371/journal.pone.0204844