Mirko Lange, Lidia Chitimia-Dobler, Gerhard Dobler
Key points
- Tick borne encephalitis came to the attention of human medicine in the 1920s and 1930s due to economic and political changes in Far Eastern Russia and Central Europe.
- Russian scientist identified the TBEV in Far Eastern Russia in the 1930s.
- Czechoslovak scientists in the late 1940s were the first to detect TBEV in Central Europe.
- In the 1960s and 1970s the transmission cycle of TBEV was elucidated mainly by Czechoslovakian and Austrian scientists.
- First trials to protect exposed humans by vaccination started shortly after the discovery of TBEV in Far Eastern Russia.
- In Austria and Germany currently used, cell culture based TBEV vaccines were developed in the 1970s and 1980s.
Tick-borne encephalitis (TBEV) is the most important tick-borne viral disease in humans and has increasingly shown its importance also in veterinary medicine. Although TBE virus (TBEV) probably evolved several thousand years ago, it was only due to political and economical changes in the 1920s that it came into the focus of human medicine in two independent locations on the European-Asian landmass. The history of TBE therefore is also a history of studying and understanding the connection of ecology of naturally occurring microorganisms and their interplay with vectors and hosts and their connection to the epidemiology of human and animal disease and underscores the importance of understanding these interrelationships for a better understanding and prevention and control of vector-borne zoonoses.
Introduction
Tick-borne encephalitis (TBE) is one of the most important arthropod-borne viral infections in Europe and Asia. Ecologically, TBE virus (TBEV) is an arbovirus. Taxonomically, it belongs to the Flavivirus genus, together with other medically relevant arboviruses such as dengue and yellow fever viruses.1 TBEV is endemic in Europe and Asia and circulates between its principal vectors, hard ticks (Ixodidae; mainly of the genus Ixodes, and small mammals (reservoir hosts). Human infection most commonly occurs through the skin via the bite of a tick. Several thousands of people are affected by TBE every year. In the literature, the first cases were assumed to be mentioned in church records from the Åland Islands (Finland) in the 18th century.2 This was long before two scientists, Smith and Kilbourne, discovered that ticks are vectors of pathogens.3 In the 20th century, a disease, which was referred to as “taiga encephalitis” or “biphasic encephalitis”, was described in soldiers, railway workers and woodcutters in the eastern parts of the former Soviet Union (USSR; see Chapter 3a).
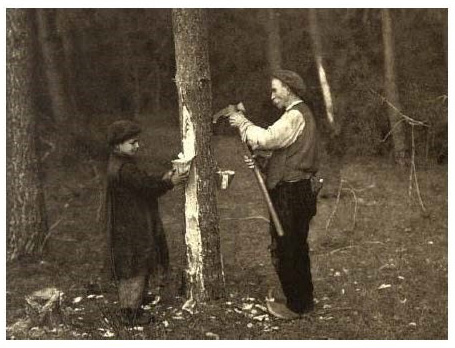
In 1931, Schneider wrote the first detailed medical description of what is today known as TBE.4 In a monograph that was published in 1932, he described more than sixty cases of “epidemic acute meningitis serosa”. Forest workers were mainly affected. As a result, TBE ultimately became the first disease that was recognised as an occupational disease in Austria, where it was known as the resin workers’ disease or Schneider’s disease. The first detailed description of the clinical picture of “summer encephalitis” in the Russian Far East was published by Panov in 1938.5
This chapter provides a brief historical overview of TBE in Europe and Asia and of the most important developments in TBE and TBEV research.
The discovery of TBEV in Europe and Asia
Based on molecular biological data, it can be assumed that western Siberia (Russia) is the area of origin of the TBEV. These scientific data also indicate an origin of this virus approximately 3100 [1800–4900] years ago.6 Whereas the eastern TBEV groups spread from western Siberia through Asia eastward, the western TBEV groups dispersed westward and may have arrived in (central) Europe approximately 2000 years ago.
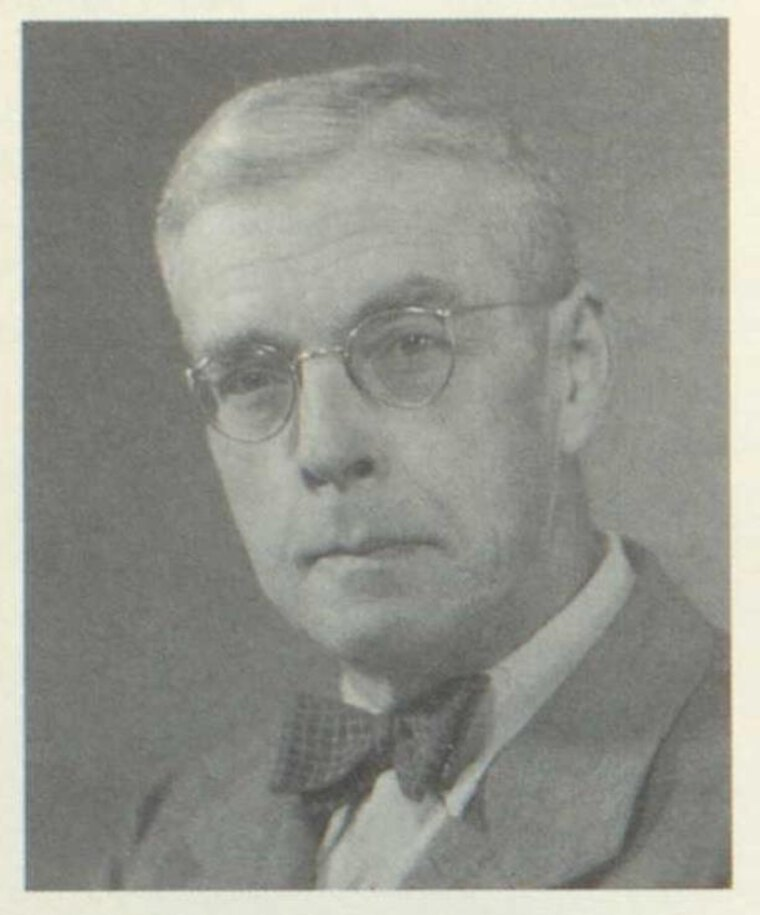
In Europe, the first medical description of four cases of what today is referred to as TBE was provided in 1931 by Hans Schneider, a physician in Lower Austria. Hans Schneider (born under the name Johann Schneider) studied medicine at the medical faculty of the University of Vienna from 1911 to 1918. During his course of study, he received two scholarships in 1912. The first scholarship was granted by the Imperial-Royal Landwehr Command in Vienna and the second by the Theobald Uffenheimer Scholarship Foundation. After having passed his final oral examination, Schneider was awarded a degree in medicine on 31 January 1919. During World War I, he joined the Imperial and Royal Army and served time with the elite Hoch- und Deutschmeister Regiment. He was awarded the Silver Medal for Bravery 1st Class (1916), the Karl Troop Cross (1916), and the Austrian Red Cross Silver Medal for his work in internal medicine (1917). From 1919 to 1924, Schneider worked as a resident at the Vienna-Lainz hospital. During this time, he familiarised himself with the most modern diagnostic procedures available at the time. This applies in particular to the early stages of clinical microbiological and serological diagnostic techniques. This was when he published his first scientific papers. In 1925, when there were severe influenza and typhoid epidemics, he was appointed as a specialist in infectious diseases to a hospital in Neunkirchen, the capital of a district in Lower Austria. In 1926, Schneider became the head of the medical department and in particular of the infectious diseases ward that was being set up. As a chief physician in internal medicine, Schneider increasingly focused on diseases of the at that time increasingly important petrochemical industry and documented all cases of workers in this industry meticulously. In 1927, he observed an epidemic increase of a usually benign form of “acute serous meningitis” and detected an association between this disease and resin tapping, which was the basis of petrochemical industry in the area south of Vienna at that time. He found that a special type of meningitis often occurred in resin tappers who harvested resin from black pines.
In his experiments, Schneider even sent clinical materials of patients (cerebrospinal fluid) to the Vienna University to infect monkeys, which, however, in contrast to poliomyelitis, which was causing similar symptoms, did not cause disease in the animals. Schneider was thus able to clearly differentiate this disease from poliomyelitis, which too was widespread at the time. Within only three years, he documented more than sixty cases of this specific disease and provided first evidence of the possibility of milk-borne transmission at that time. In 1931, Schneider reported on four cases in the Wiener Klinische Wochenschrift and thus provided the first detailed clinical description of the disease worldwide. In 1932, he published a comprehensive monograph on “Epidemic acute meningitis serosa”, in which he described a total of 66 cases from the years 1927 to 1931 and presented his studies on the differentiation of this disease from other infectious diseases (poliomyelitis, typhoid fever). Owing to Schneider’s propaedeutic skills, this previously unknown disease was recognised as a new infectious disease that was associated with resin tapping. TBE was the first disease that was recognised as an occupational disease in Austria (where it was known as the resin workers’ disease). It was not until Schneider’s death in 1954 that this new entity became known, especially in German-speaking areas, as Schneider’s disease, named after the person who first described it.7
Figure 2: Dr. Johann (Hans) Schneider (1891 – 1954)
(Source: Niederösterreichische Ärztechronik – Geschichte der Medizin und der Mediziner Österreichs, Wien: Verlag Oskar Möbius GmbH 1990; S. 695 – 696: Nr. 20.)
In the Soviet Far East taiga, a severe and usually fatal neurological disease was observed in 1934 and 1935 among Red Army soldiers who were stationed in this area and among the local population (see also chapter 3a). First attempts to identify the causative agent were unsuccessful and the etiology of the disease was unknown. In 1937, an expedition team led by Professor Lev Aleksandrovich Zilber (head of the first medical virology laboratory in the USSR) and Professor Evgenyi Nikanorovich Pavlovsky was sent to the taiga region on behalf of the Soviet health ministry in order to investigate the cause of the disease. Pavlovsky did not personally participate, but four scientists from his institute took part in this first expedition. The team of specialists (scientists and technical assistants) was divided into two groups. The first group investigated the Khabarovsk territory in the north and the second group the Primorsky territory in the south. In spite of extremely difficult conditions in remote areas (absence of infrastructure), the teams found that many local people showed neurological symptoms. Of 64 patients who were treated in a hospital, 12 died. The virus was isolated from 29 patient samples.8-11
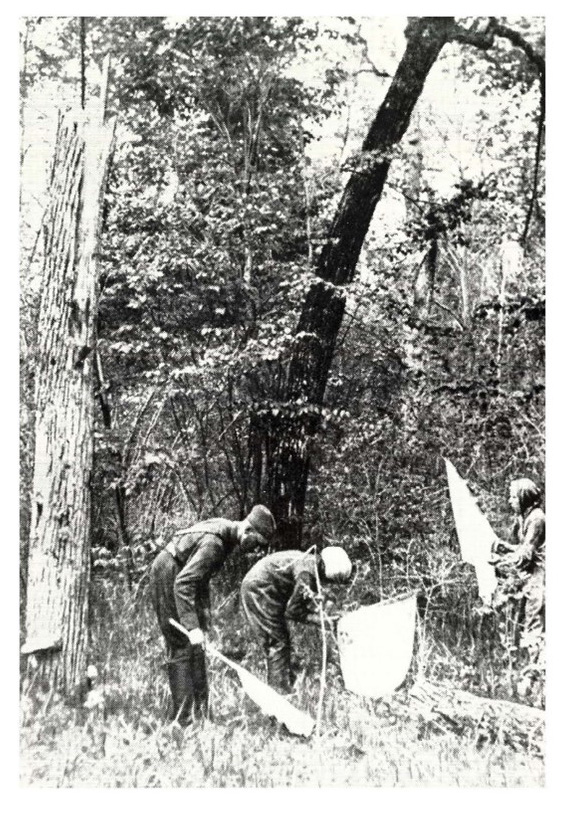
Figure 3: Diffuse biotope of the ticks Ixodes persulcatus, Haemaphysalis japonica and H. concinna in the taiga
(Source: [Natural nidality of transmissible diseases with special reference to the landscape epidemiology of zooanthroponoses]. Moscow, Leningrad: Nauka (in Russian). 1966)
In order to prevent infection, the teams informed the local population about the potential hazards associated with ticks. As a result, the number of new cases was significantly reduced within a short period of time. At the end of their mission, Zilber and his expedition team were able to provide convincing results suggesting that they had identified the causative virus and its vector (Ixodes persulcatus).
Some team members became infected with TBEV during the mission and showed typical disease symptoms. Since the virus is highly contagious and the conditions were challenging, it was almost a miracle that none of the affected team members died from the disease. Dr Chumakov, for example, became infected with the virus after having cut his finger during an autopsy. After a short while, he developed first symptoms such as paralysis of his right arm and loss of hearing. Later in his scientific career, Chumakov became a highly esteemed virologist and discovered TBEV foci at a great distance from the Far East in the Ural and Trans-Ural regions.12
On the whole, the first expedition under the direction of Lev A. Zilber was a success and a major scientific achievement. During this mission, the team successfully isolated the virus several times, worked out the epidemiology of the disease, and took measures to prevent further infections. Owing to this success, it is no surprise that other expedition teams led by Evgenyi N. Pavlovsky were sent to the Far East in order to gather more information on the disease and especially on the virus.13
In Europe, the first isolation of TBEV was achieved in Belarus in 1939 from Ixodes ricinus ticks.14 In the People’s Republic of China, the first cases were reported in 1943. The virus was isolated for the first time from brain samples from deceased patients in 1944 (review by Yoshii et al., 2017).15 In the early 1940s, US scientists at the Rockefeller Institute for Medical Research detected cross-reactivity between hyperimmune sera of Louping ill virus and Russian spring-summer encephalitis virus.
As early as in 1948, the second virus isolation (Hanzalova strain) was achieved in Europe in the present-day Czech Republic (near Prague).16 The early 1950s played a special role in the history of TBE. In 1952, only a few years after the first virus isolation, a strain that was named “KEM I” was isolated in Hungary. Virus isolations were also achieved in Slovenia in 1953 and in Poland in 1954. In 1954, the first cases of TBE were reported on the island of Bornholm (Denmark). In the same year, TBEV was detected for the first time in Sweden. In Austria, the first TBEV isolates came from Styria in collaboration with Czechoslovak scientists in 1953. The Scharl strain, an isolate form the brain of a fatal human case, was isolated in Vienna, Austria in 1954. In 1958, the virus was detected for the first time in Slovakia. The Kumlinge strain was isolated in Finland in 1959.17,18 In divided Germany, the first virus isolation was achieved by scientists in the German Democratic Republic in the late 1950s.19 In addition, the first case of TBE in Norway was reported as late as 1997.20 In 2020, the virus and human cases were documented for the first time in the British Isles.21 Two years later, TBEV was detected for the first time outside of Europe and Asia on the African continent (Tunisia).22
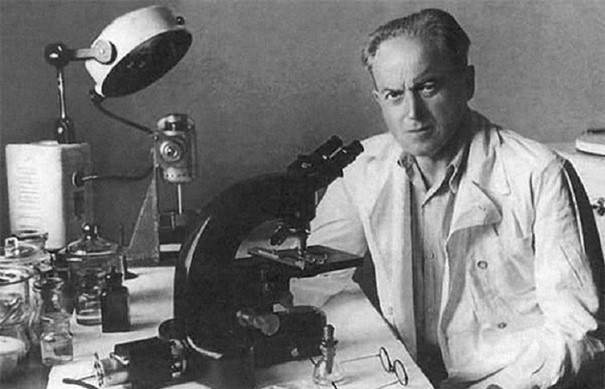
Figure 4: Prof. Dr. Lev Alexandrovich Zilber (1894 – 1966)
(Source: “Lev Alexandrovich Zilber” written by his son L.L. Kisselev and E.S. Levina, The Publishing House “Science”, Series “Scientific biographies”)
In the Federal Republic of Germany, the Zimmern TBEV strain was isolated for the first time in the region of Lower Franconia in 1970.23, 24 French scientists successfully isolated a TBEV strain in Alsace in 1970.25 It was only in 2016 that the Netherlands reported the first autochthonous cases of TBE and the successful isolation of the Sallandse TBEV strain.26
The detection and natural transmission cycle of TBEV
The first expedition to the Russian Far East was led by Zilber in 1937 and provided first important information on the eco-epidemiology of TBEV within a few months. The causative agent was found to be a virus that was transmitted to a human host via the bite of an Ixodes persulcatus tick (Ixodidae family).
As mentioned before, the first expedition was followed by two further expeditions to the Russian Far East under the direction of Professor Evgenyi Nikanorovich Pavlovsky, who also was a general in the Red Army. The purpose of the second expedition (1938) was to investigate the spread of TBEV in the field and to identify the reservoir hosts of the virus. The results of the expedition were incorporated into Pavlovsky’s widely acclaimed ideas about the ecology of zoonotic diseases (Natural Nidality of Transmissible Diseases).27, 28 TBEV is transmitted from a natural (transmission-competent) reservoir host to a vector (Ixodes ticks) through a blood meal. Infected vectors may transmit the virus to their accidental hosts (humans) during the next blood meal through the skin via a bite. These reservoir hosts are infected via the bite of an infected tick and transmit the virus to other ticks feeding on the host’s blood. Long-term circulation of the virus depends on the presence of all necessary biotic factors (vectors, hosts) and an appropriate abiotic environment.
The scientists Chumakov and Naidenova29 found that Ixodes ricinus, which is related to Ixodes persulcatus, is a vector that transmits a milder form of TBE in some European regions of the former USSR. This description was later confirmed by several European researchers (e.g. from Belarus and the former Czechoslovakia).In the former Czechoslovakia, Rampas and Gallia were the first outside of the USSR to isolate TBEV from field-collected ticks.30-32
From 1947 to 1951, a different route of transmission of TBE to humans was observed in the European part of the former Soviet Union.33 TBEV was found to be transmitted through the ingestion of unpasteurised milk or milk products (e.g. cheese) from viraemic goats. One of the largest epidemics outside of the USSR occurred in the southeastern part of Slovakia (including the town of Rožňava) in 1951. More than 600 cases were documented.34 Ten years later, cases resulting from alimentary transmission were reported in the former German Democratic Republic (e.g. in the town of Niesky).35
The 1970s and 1980s witnessed a substantial decrease in field work in many European countries. Since the ecology of TBEV had been well studied and understood by the scientific community, the focus of research attention shifted to molecular biological studies of TBEV and to Borrelia burgdorferi, a newly identified causative agent of Lyme disease. It is interesting to note that this coincided with the time when the first European vaccine became available in 197636 and it was believed that all problems associated with TBE had been solved. Today we know that this assumption was wrong.
Jones et al.37 found that guinea pigs acquired Thogoto virus through Rhipicephalus appendiculatus ticks but did not develop detectable levels of virus in their blood. Alekseev and Chunikhin38 as well as Labuda et al.39 demonstrated the non-viraemic transmission of TBEV from small mammals to uninfected blood-feeding ticks. This was an important contribution to the understanding of the field ecology of the virus, and TBEV ecology once again became a focus of scientific attention. Milan Labuda et al.40-42 found that (a) TBEV was transported in Langerhans cells of infected hosts, (b) non-viraemic transmission was also possible in immune hosts, and (c) this type of transmission occurred in small mammals but not in large mammals. This non-viraemic transmission now is more commonly referred to as infection by co-feeding.
The detection of different TBEV subtypes
On the basis of its general characteristics (physical and chemical properties, virion structure, arthropod carriers, and cross-reactivity), the Flavivirus genus was considered to belong to the Togaviridae family. This term was first used by Lwoff and Tournier in 1966.43
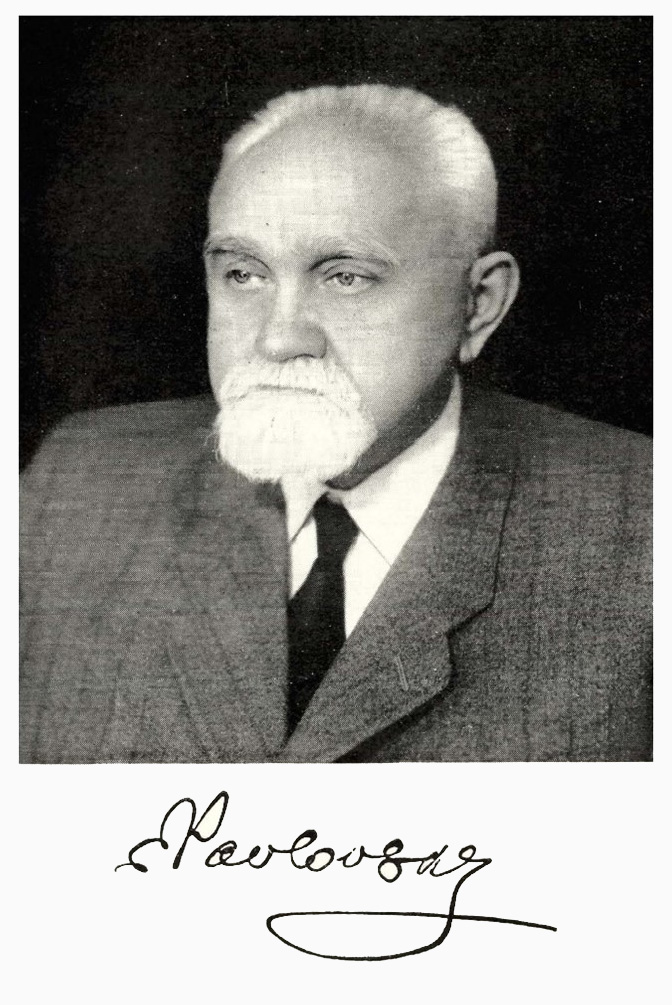
Figure 5: Prof. Dr. Evgenyi Nikanorovich Pavlovski
(J. N. Pawlowski – Leben und Werk, Berlin: VEB Deutscher Verlag der Wissenschaften 1959)
The Togaviridae family included the Alphavirus genus (formerly Group A arboviruses) and flaviviruses (formerly Group B arboviruses). Group B included dengue virus type 1 and other viruses. 44, 45 Based on the plaque reduction neutralisation test (PRNT) and virus structure and viral replication, it was recognized that the former family of Togaviridae comprised two completely different groups of viruses. These finally were divided into two families, the genus Alphavirus in the family Togaviridae, and the newly created family Flaviviridae. This newly created genus, now called Orthoflavivirus in family Flaviviridae was further divided according to cross neutralization into seven subgroups.46 One of these subgroups, the so-called “Tick-borne flavivirus group” contain the mammalian tick-borne flavivirus group (among others TBEV, Omsk haemorrhagic fever virus, Louping ill virus, Langat virus, Powassan virus, and Kyasanur Forest virus) and the Seabird tick-borne flavivirus group (among them Gadgets Gully virus, Saumarez, Reef virus, and Tyuleniy virus).
Although all these viruses have similarities, there are differences between them in their geographical distribution, associations with different vertebrates and ticks, and pathogenicity for humans. The Flaviviridae family comprises more than 70 species and includes ten sero-complexes.48 TBEV belongs to the group of flaviviruses, which are mainly transmitted by ticks feeding on the blood of mammals. It has three subtypes: European, Far Eastern and Siberian.49
Two geographic and antigenic TBEV variants (eastern and western) have been known for more than 40 years.1,50-51 Clarke52 divided 28 strains into two antigenic variants using the gel precipitation test with cross-absorbed sera and found that there were two types of antigens: eastern and western (European). Chumakov et al.53 believed that there were differences between the Eastern and Western subtypes of TBEV and proposed a classification into the antigenic variants “persulcatus” and “ricinus” depending on viral ecology. Votyakov et al.54,55 emphasised differences in antigenic profiles, geography, and clinical and pathological features in animals and humans.
Pletnev et al. 56,57 and Mandl et al. 58,59 decoded the whole genomes of Eastern (Sofjin) and European (Neudoerfl) subtype TBEV strains. This was the beginning of a new phase of the genetic classification of TBEV. Data showed significant genetic differences between the Western and Eastern variants in nucleotide substitutions (16.8–16.9%) and amino acid substitutions (6.9–7.2%). Also two Eastern strains were found to differ significantly in nucleotide (4.6%) and amino acid (1.8%) substitutions.
Rubin and Chumakov60 were the first to publish these results for the Siberian subtype and, for example, described the isolation of a TBEV strain (Aina) from a child in the Irkutsk region (USSR). Pogodina et al. 61, 62 reported the isolation of a group of strains from Ixodes persulcatus in eastern Siberia. These strains are serologically related to the Aina strain. Gritsun et al.33, 63 and Zlobin et al.64-66 provided the first genotypic characterisation of what is today known as the Siberian subtype by sequencing the E gene and then the whole genome.
Sequencing a gene E fragment of eight and then 29 strains that were isolated in different geographical regions allowed the three major subtypes (Far Eastern, Western and Ural-Siberian) to be identified. Ecker67 believed that there were three TBEV subtypes corresponding to the three major genotypes. Grard,68 however, provided a new interpretation of the genetic relationships between arthropod-borne viruses and proposed that TBEV be divided into four subtypes: (1) Louping ill virus (Spanish, British and Irish subtypes), (2) Western TBEV (European subtype), (3) Eastern TBEV (Far Eastern and Siberian subtypes), and (4) Turkish sheep encephalitis virus, including the Greek goat encephalitis virus subtype.
In addition to the three known and accepted subtypes, Russian researchers described two further strains that were denoted as 178/79 and 886/84. They proved that these two Russian strains were not closely related to the other three subtypes. The latter strain with a number of isolated is now accepted as a fifth subtype of TBEV, named Baikalian subtype. The classification of the 178/79 strain is rather unclear as only on single isolate so far exists.69 Further studies are required to assess whether these two new strains can be classified as further TBEV subtypes.
The development of TBEV vaccines
Pavlovsky was a pioneer in the development of a TBEV vaccine. A TBEV vaccine derived from mouse brain was for the first time administered to the local population in 1939 during the third expedition, which was led by E. N. Levkovich and N. L. Dankovsky. In 1940, mass vaccination was carried out for the first time in the Russian Far East (Khabarovsk) under the direction of Elizaveta Nikolaevna Levkovich.70
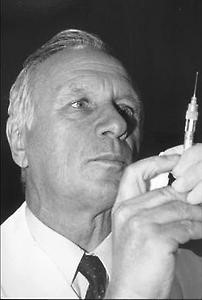
In order to address the increasing medical importance of TBE in Austria, Professor Christian Kunz decided to develop a vaccine against TBE. For this purpose, he cooperated with the British biological warfare research centre at Porton Down. This was possibly a result of many years of cooperation with the US armed forces. This cooperation was of utmost importance to Kunz since zonal ultracentrifugation, a purification method which was absolutely necessary for the production of vaccines, was available at this research facility. Kunz administered the first two TBE vaccines to himself and to his colleague Professor Hanns Hoffmann, a virologist. He carried out the first major vaccination campaigns and tested the vaccine on approximately 30,000 farmers and forest workers in Austria. He was personally liable for these activities. His private liability insurance covered 10 million schillings (approximately € 720,000).71
Kunz was unable to convince some of the major vaccine manufactures to become a partner in vaccine production. In 1976, the founders of IMMUNO AG, an Austrian pharmaceutical company, joined the project and started mass production of the vaccine (FSME-Immun®). Since then, 85% of the Austrian population have been vaccinated and the number of TBE cases in Austria has been reduced by approximately 90%. It should be noted that vaccination rates have been decreasing in Austria over the years as a result of a lack of acceptance in society. In 1991, another TBE vaccine (Encepur®) was approved in various European countries. This vaccine had been developed by the German pharmaceutical company Behringwerke and was then supplied by Chiron Corporation after the latter had acquired the vaccine businesses of Behringwerke.71
Professor Franz Xaver Heinz, director of the Institute of Virology in Vienna, and his team discovered a new mechanism of membrane function between virus and cellular membranes, a mechanism which is unique to flaviviruses. He was also the first to determine the three-dimensional structure of the envelope protein E. Heinz and his research group thus enhanced the existing knowledge about fundamental mechanisms in virology. These scientific discoveries provided the molecular basis for many aspects of TBE immunology and pathogenesis.
TBE has become an important model for studying different cellular and virological mechanisms. In addition, this was also the time when the first infectious clone of TBEV was constructed allowing comprehensive studies on the genetics of TBEV.72 Due to the nature of TBE as a zoonosis it will probably not be possible to extinguish this disease from our world. TBE will stay a permanent medical problem in Europe, Asia and probably will also expand its importance to Africa in the near future, as the TBEV was detected there, recently. In many of the endemic regions in Europe, there is an increasing trend of human TBE cases, even in highly vaccinated populations, like in Austria. The reason for this development has so far not understood, but may be related to the massive changes in global, regional and local ecological and environmental interactions due to human activities. Therefore, the prevention of TBE in humans and animals will remain a challenge although all instruments for control of human disease have been provided in the past by many brave, innovative and engaged researchers from different countries which faced the same problems although coming from political and economic suppositions.
Figure 7: Franz Xaver Heinz
(Franz X. Heinz mit Loeffler-Frosch-Medaille ausgezeichnet; meduniwien.ac.at)

Contact
Citation
Lange M, Chitimia-Dobler L, Dobler G. Short History of TBE Research and the Scientists behind it. Chapter 3b. In: Dobler G, Erber W, Bröker M, Chitimia-Dobler L, Schmitt HJ, eds. The TBE Book. 7th ed. Singapore: Global Health Press; 2024. doi:10.33442/26613980_3b-7
References
- Casals J. Viruses: the versatile parasites; the arthropod-borne group of animal viruses. Trans N Y Acad Sci. 1957;19:219-35.
- Kunz C, Heinz FX. Tick-borne encephalitis. Vaccine. 2003;21Suppl 1:S1-2.
- Smith T, Kilbourne FL. Investigations into the nature, causations and prevention of Texas or southern cattle fever. Bureau Anim Ind Bull. 1893:322pp.
- Schneider H. Über epidemische akute Meningitis serosa. Wiener Klin Wochenschr. 1931;44:350-2.
- Panov AG. Klinika vesenne-letnikh entsefalitov. Nevropat I Psikhiat. 1938;7:18-32.
- Heinze DM, Gould EA, Forrester NL. Revisiting the clinal concept of evolution and dispersal for the TB flaviviruses by using phylogenetic and biogeographic analyses. J Virol. 2012;86:8863-71.
- Lange M, Chitimia-Dobler L, Dobler G. Dr. Hans (Johann) Schneider – Medical Officer and First Describer of Tick Borne Encephalitis. WMM 2021; 65(8): 294-301. doi 10.48701/opus4-51.
- Pavlovskij EN., 1964. [Natural nidality of transmissible diseases with special reference to the landscape epidemiology of zooanthroponoses.] Moscow, Leningrad: Nauka. (in Russian) (engl. transl. 1966, edited by N.D. Levine, University of Illinois Press, 257 pp.).
- Pavlovskij EN., 1966. [Natural nidality of transmissible diseases in relation to landscape epidemiology of zooanthroponoses.] Moscow, Leningrad (in Russian) (engl. transl. 1966, edited by Y. Shirokov, Peace Publishers).
- Pavlovsky YN. Human Diseases with Natural Foci. Moscow, UdSSR. Foreign Languages Publishing House. 1963
- Borchert A. J. N. Pawlowski Leben und Werk. Berlin. VEB Deutscher Verlag der Wissenschaften. 1959
- Chumakov MP, Seitlenok NA. Tick-borne human encephalitis in the European part of USSR and Siberia. Science. 1940;92:263-4.
- Zlobin VI, Pogodina VV, Kahl O. A brief history of the discovery of TBE virus in the late 1930s (based on reminiscences of members of the expeditions, their colleagues, and relatives). Ticks Tick Borne Dis. 2017;8:813-20.
- Chumakov MP. Tick-borne encephalitis in humans. PhD of Med Sci. Moscow, 1944 [In Russian].
- Yoshii K, Song JY, Park SB, Yang J, Schmitt HJ. Tick-borne encephalitis in Japan, Republic of Korea and China. Emerg Microbes Infect. 2017; 6(9):e82
- Gallia F, Rampas J, Hollender L. Laboratory infection with encephalitis virus. Cas Lék Ces. 1949;88:224-229 [In Czech].
- Oker-Blom N, Kääriäinen L, Brummer-Korvenkontio M, Weckström P. Symp. Czech. Acad. Sci. 1962;3:423. (cited after Brummer-Korvenkontio et al., 1973)
- Brummer-Korvenkontio M, Saikku P, Korhonen P, Oker-Blom N. Arboviruses in Finland. I. Isolation of tick-borne encephalitis (TBE) virus from arthropods, vertebrates, and patients. Am J Trop Med Hyg. 1973;22:382-9.
- Sinnecker H. Zeckenencephalitis in Deutschland. Zbl Bakt., I. Abt Orig. 1960;180:12-18.
- Skarpaas T, Ljøstad U, Sundøy A. First human cases of tickborne encephalitis, Norway. Emerg Infect Dis. 2004;10:2241-3.
- Holding M, Dowall SD, Medlock JM, Carter DP, Pullan ST, Lewis J, Vipond R, Rocchi MS, Baylis M, Hewson R. Tick-Borne Encephalitis Virus, United Kingdom. Emerg Infect Dis. 2020 Jan; 26(1):90-96.
- Fares W , Dachraoui K, Cherni S, Barhoumi W, Ben Slimane T, Younsi H, Zhioua E. Tick-borne encephalitis virus in Ixodes ricinus (Acari: Ixodidae) ticks, Tunisia. Ticks Tick Borne Dis. 2021 Jan;12(1):101606.
- Rehse-Küpper B, Danielová V, Klenk W, Abar B, Ackermann R. The isolation of Central European encephalitis (Tick-borne encephalitis) virus from Ixodes ricinus (L.) ticks in southern Germany. Zbl Bakt Hyg., I. Abt Orig. A 1978;242:148-155.
- Müller W, Löffler S, Preis B. Experimentelle Untersuchungen über das Vorkommen von Arboviren in Unterfranken. II. Charakterisierung zweier Virusstämme. Zentralbl Bakteriol Orig. 1970;214:465-479.
- Hannoun C, Chatelain J, Krams S, Guillon JC, Lepine P. Isolement, en Alsace, du virus de l’encephalite à tiques (Arbovirus, groupe B). C R Acad Sci. Paris. 1971;272:766-8.
- de Graaf JA, Reimerink JH, Voorn GP, et al. First human case of tick-borne encephalitis virus infection acquired in the Netherlands, July 2016. Euro Surveill. 2016;21.
- Pavlovsky EN. On the natural focality of infectious and parasitic diseases. Vestn. Akad. Nauk SSSR 1939;10:98–108 [In Russian].
- Pavlovsky EN. Natural Nidality of Transmissible Diseases: With Special Reference to the Landscape Epidemiology of Zooanthroponoses. University of Illinois Press; 1966.
- Chumakov MP, Naidenova GA. The tick Ixodes ricinus as a vector of the tick-borne (spring-summer) encephalitis. Med Parazitol. Parazit Bolezni. (Moscow) 1944;4:89-93 [In Russian].
- Blaškovič D. The public health importance of tick-borne encephalitis in Europe. Bull WHO. 1967;36(suppl 1):5-13.
- Rampas J, Gallia F. The isolation of encephalitis virus from Ixodes ricinus. Cas Lek Ces. 1949;88:1179-1180.
- Hubàlek Z. History of Arbovirus Research in the Czech Republic. Viruses 2021, 13, 2334, 1-34. https://doi.org/10.3390/v13112334.
- Gritsun TS, Lashkevich VA, Gould EA. Tick-borne encephalitis. Antiviral Res. 2003;57:129-46.
- Ruzek D, Kaucka K. A brief tale of two pioneering moments: Europe’s first discovery of Tick-Borne Encephalitis (TBE) virus beyond the Soviet Union and the largest alimentary TBE outbreak in history. Ticks and Tick-borne Diseases 15 (2024) 102314
- Helpert A, Sinnecker H. Ausgewählte Erhebungen zur Zeckenenzephalitis-Epidemie im Kreis Niesky, Bezirk Dresden, 1961. Deutsch Gesundheitsw. 1966;21:1277-9.
- Kunz C. Vaccination against TBE in Austria: the success story continues. Int J Med Microbiol. 2002;291 Suppl 33:56-7.
- Jones LD, Davies CR, Steele GM, Nuttall PA. A novel mode of arbovirus transmission involving a nonviremic host. Science. 1987;237:775-7.
- Alekseev AN, Chunikhin SP. The exchange of the tick-borne encephalitis virus between ixodid ticks feeding jointly onanimals with a subthreshold level of viremia. Parazit Bolezni. (Moscow). 1990:48-50 [In Russian.]
- Labuda M, Jones LD, Williams T, Danielova V, Nuttall PA. Efficient transmission of tick-borne encephalitis virusbetween cofeeding ticks. J Med Entomol. 1993;30:295-9.
- Labuda M, Austyn JM, Zuffova E, et al. Importance of localized skin infection in tick-borne encephalitis virus transmission. Virology. 1996;219:357-66.
- Labuda M, Kozuch O, Zuffova E, Eleckova E, Hails RS, Nuttall PA. Tick-borne encephalitis virus transmission between ticks cofeeding on specific immune natural rodent hosts. Virology. 1997;235:138-43.
- Nuttall PA, Labuda M. Tick-borne encephalitis subgroup. In: Ecological Dynamics of Tick-borne Zoonoses. Eds SonenshineDE, Mather TN: Oxford University Press; 1994;pp.351-391.
- Lwoff A, Tournier P. The classification of viruses. Annu Rev Microbiol. 1966;20:45-74.
- Fenner F, McAuslan BR, Mims CA. The Biology of Animal Viruses. New York – London: Academic Press; 1974.
- Horzinek M. Togaviruses. Ann Med Vet. 1978;122:293-9.
- De Madrid AT, Porterfield JS. The flaviviruses (group B arboviruses): a cross-neutralization study. J Gen Virol. 1974;23:91-6.
- Gaidamovich SY, Loginova NV. Family Togaviridae. In: General and Particular Virology, Moscow: Medicina. 1982;2:520pp [In Russian].
- Westaway EG, Brinton MA, Gaidamovich S, et al. Flaviviridae. Intervirology. 1985;24:183-92.
- Thiel H-J, Collett MS, Gould EA, et al. Family Flaviviridae. In: Virus Taxonomy: Classification and Nomenclature. Eighth Report of the International Committee on the Taxonomy of Viruses. Eds Fauquet CM, et al. Amsterdam: Elsevier; 2005;979-996
- Chumakov MP. Investigations on ultraviral encephalitides. VI. Transmission of tick-borne encephalitis virus to the progeny of ixodid ticks and the problem of natural reservoirs of this infection. Med Parazit (Moscow). 1944;6:38 [In Russian].
- Clarke DH. Antigenic analysis of strains group B arthropod-borne viruses by antibody absorption. J Exp Med. 1960;1: 21-32.
- Clarke DH. Further studies on antigenic relationships among the viruses of the group B tick-borne complex. Bull WHO. 1964;31:50-66.
- Chumakov MP, Rubin SG, Linev MB. Three antigen types of tick -borne encephalitis virus, their dependence on arthropodvectors and geography. Problems of Medical Virology (Мoscow). 1975:371-5 [In Russian].
- Votyakov VI, Protas II, Zhdanov VM. Western tick-borne encephalitis. Minsk: Belarus; 1978;255 pp. [In Russian].
- Votyakov VI, Zlobin VI, Mishayeva NP. Tick-borne encephalitis of Eurasia: Ecology, Molecular epidemiology, Nosology and Evolution. Novosibirsk Nauka. 2002 [In Russian].
- Pletnev AG, Yamshchikov VF, Blinov VM. Tick-borne encephalitis virus genome. The nucleotide sequence coding for virion structural proteins. FEBS Lett. 1986;200:317-21.
- Pletnev AG, Yamshchikov VF, Blinov VM. Nucleotide sequence of the genome and complete amino acid sequence of the polyprotein of tick-borne encephalitis virus. Virology. 1990;174:250-63
- Mandl СW, Heinz FX, Kunz C. Sequence of the structural proteins of tick-borne encephalitis virus (western subtype) and comparative analysis with other flaviviruses. Virology. 1988;166:197-205.
- Mandl СW, Heinz FX, Stocke E, Kunz C. Genomic sequence of tick-borne encephalitis virus (western subtype) and comparative analysis of nonstructural proteins with other flaviviruses. Virology. 1989;173:291-301.
- Rubin SG, Chumakov MP. New data on the antigenic types of tick-borne encephalitis (TBE) virus. Zentralbl Bakteriol. 1980;Suppl. 9:231-6.
- Pogodina VV, Bochkova NG, Levina LS, et al. Immunological and some etiology aspects of the Aina/1448 serotype of tick-borne encephalitis virus. Voprosy Virusol. 1981;6:735-41 [In Russian].
- Pogodina VV, Bochkova NG, Koreshkova GV. Properties of strains of tick-borne encephalitis virus, Aina/1448 serotype. Voprosy Virusol. 1981:741-5 [In Russian].
- Gritsun TS, Frolova TV, Pogodina VV, Lashkevich VA, Venugopal K, Gould EA. Nucleotide and deduced amino acid sequence of the envelope gene of the Vasilchenko strain of TBE virus; comparison with other flaviviruses. Virus Res. 1993;27:201-9.
- Zlobin VI, Mamayev LV, Dzhioev YP, Kozlova IV. Genetic types of tick-borne encephalitis virus. J Infect Pathol (Irkutsk). 1996;3:13-7 (In Russian).
- Zlobin VI, Demina TV, Belikov SI, et al. Genetic typing of tick-borne encephalitis virus based on an analysis of the levels of homology of a membrane protein gene fragment. Voprosy Virusol. 2001;1:16-21 [In Russian].
- Zlobin VI, Demina TV, Mamayev LV, et al. Analysis of genetic variability of strains of tick-borne encephalitis virus by primary structure of a fragment of the membrane protein E gene. Voprosy Virusol. 2001:13-6 [In Russian].
- Ecker M, Allison SL, Meixner T, Heinz FX. Sequence analysis and genetic classification of tick-borne encephalitis viruses from Europe and Asia. J Gen Virol. 1999;80:179-85.
- Grard G, Moureau G, Charrel RN, et al. Genetic characterization of tick-borne flaviviruses: new insights into evolution, pathogenic determinants and taxonomy. Virology. 2007;361:80-92.
- Demina TV, Dzhioev YP, Verkhozina MM, et al. Genotyping and characterization of the geographical distribution of tick-borne encephalitis virus variants with a set of molecular probes. J Med Virol. 2010;82:965-76.
- Zlobin VI, Pogodina VV, Kahl O. A brief history of the discovery of tick-borne encephalitis virus in the late 1930s (based on reminiscences of members of the expeditions, their colleagues, and relatives). Ticks and Tick-borne Diseases 8 (2017) 813-820
- Dobler, G. Die FSME – eine durch Zecken übertragene Zoonose mit wehrhistorischer und wehrmedizinischer Bedeutung. WMM 2021 65(8): 302-307
- Dobler, G Gniel D. A History of Tick-Borne Encephalitis and Its Virus. In: Vasilakis N, Kramer L. D, eds. History of Arbovirology: Memories from the Field, Volume II: Virus Family and Regional Perspectives, Molecular Biology and Pathogenesis, pp. 453-467. Cham, Switzerland. Springer Nature. 2023